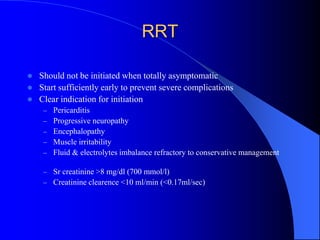
Chronic renal failure (CRF) is a progressive decline in kidney function leading to end-stage renal disease (ESRD), requiring renal replacement therapy to prevent life-threatening uremia. Causes of CRF include congenital diseases, glomerular and vascular disorders, and urinary tract obstructions, with symptoms becoming pronounced as kidney function deteriorates. Management involves addressing underlying causes, implementing dietary and pharmacological strategies, and considering renal replacement therapies like dialysis and transplantation when appropriate.