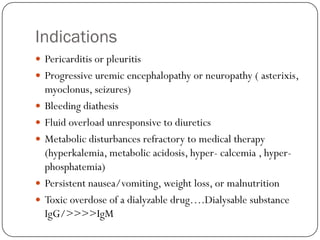
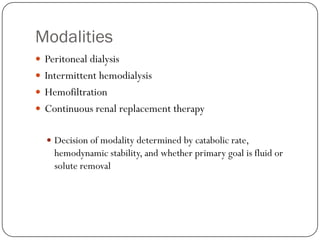
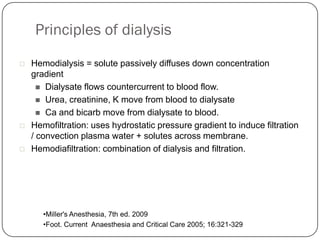
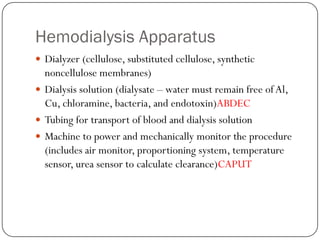
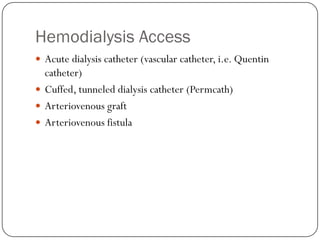
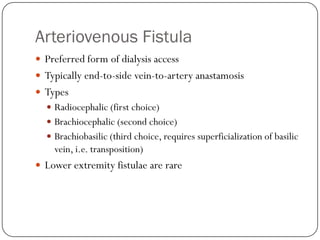
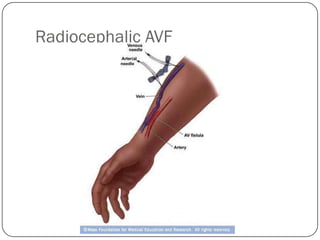
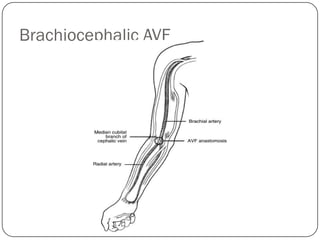
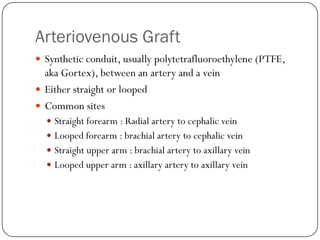
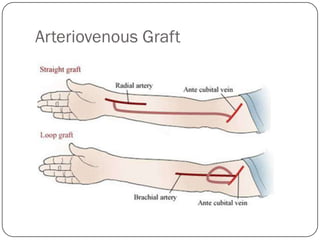
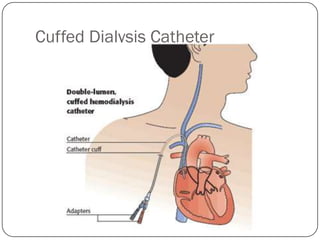
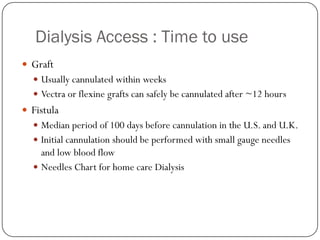
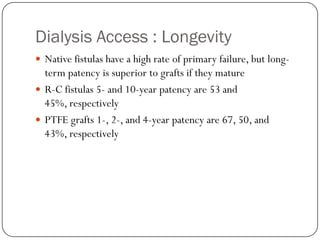
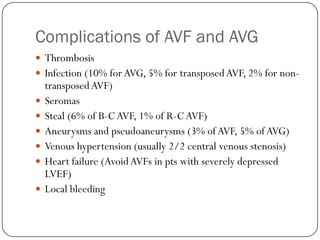
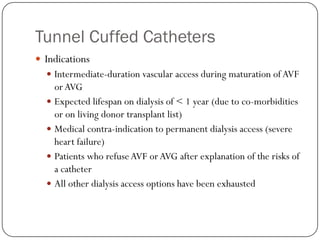
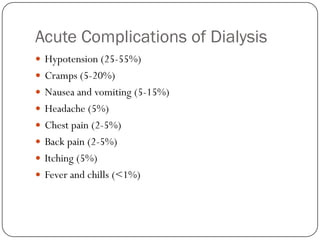
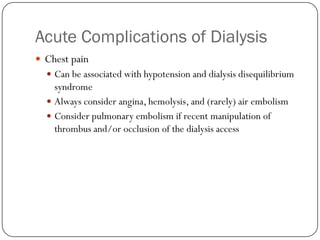
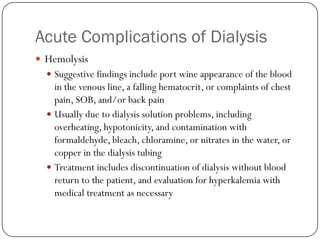
Dialysis is used to treat kidney failure and manage its complications. There are different modalities including peritoneal dialysis, hemodialysis, and continuous renal replacement therapy. Hemodialysis uses a dialyzer, tubing, and machine to remove waste and fluid by diffusion and ultrafiltration as blood and dialysate flow countercurrently. Vascular access includes catheters, arteriovenous grafts, and arteriovenous fistulas. Complications can include infections, thrombosis, and fluid overload.