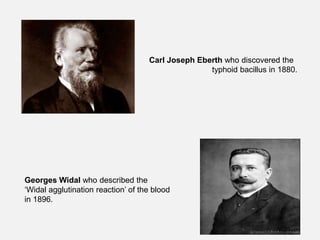
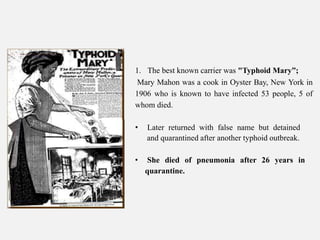
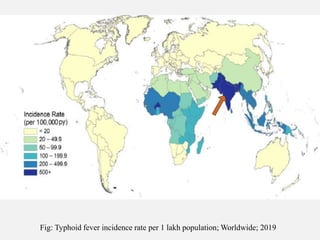
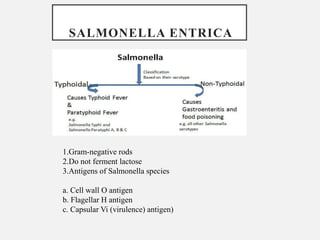
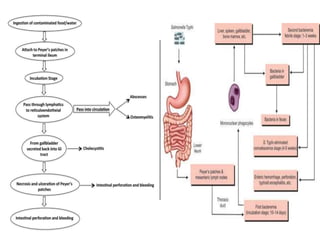
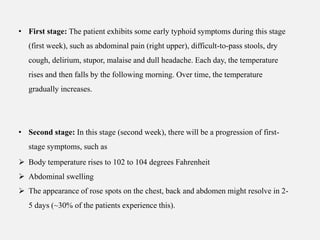
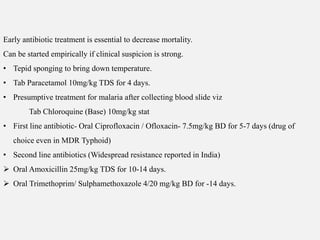
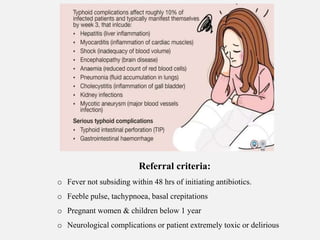
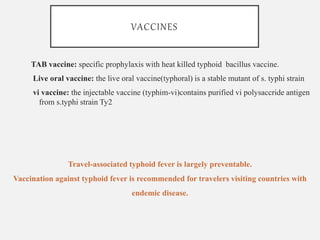
Typhoid fever, primarily caused by Salmonella typhi, is a serious infection that leads to 11-21 million cases and 135,000-230,000 deaths annually worldwide, predominantly affecting developing regions. Its symptoms progress through four stages over a week, encompassing abdominal pain, high fever, and potentially severe complications like intestinal perforation. Early antibiotic treatment and preventive measures, including vaccination, are critical to managing and controlling the disease.