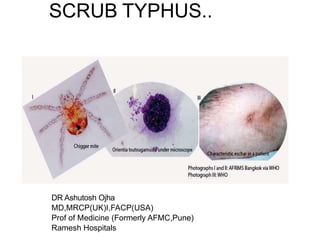
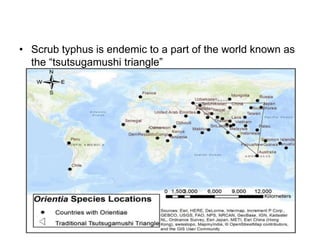
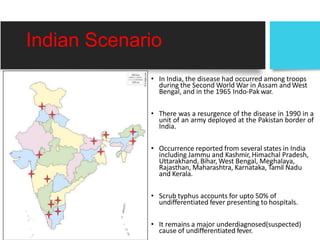
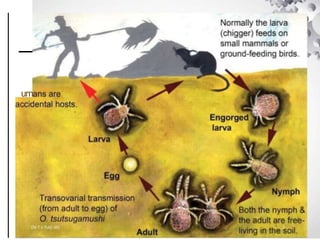
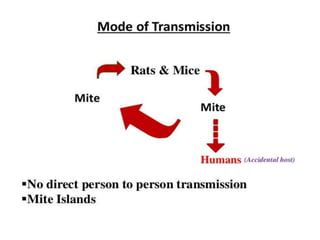
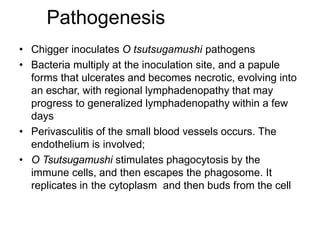
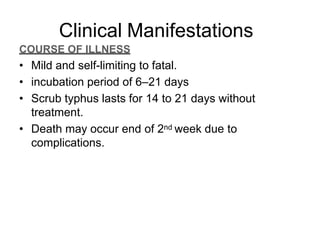
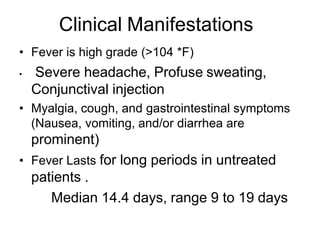
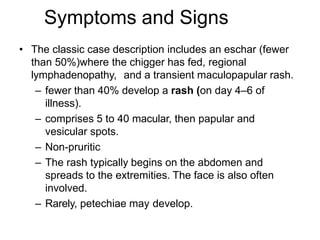
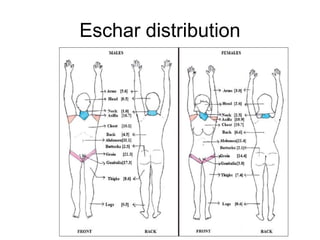
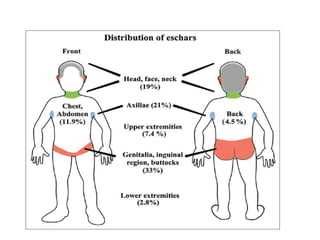
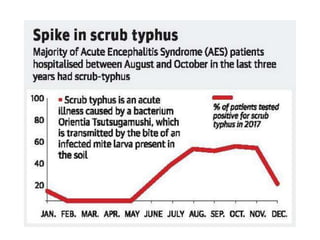
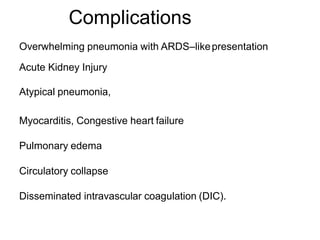
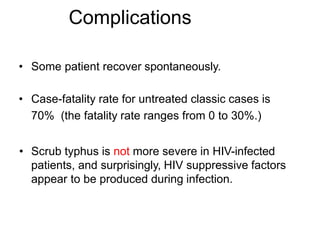
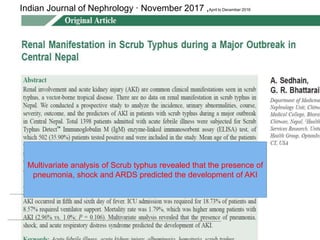
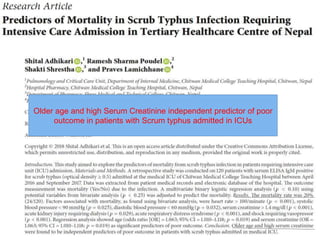
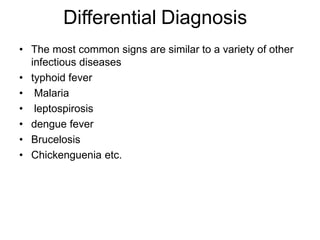
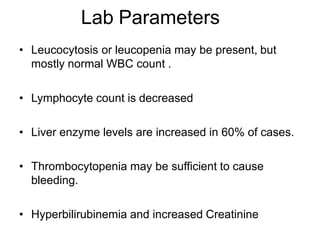
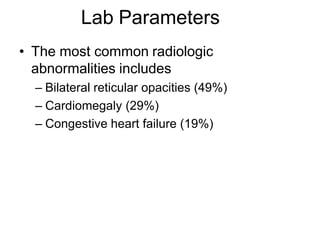
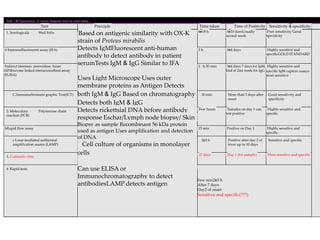
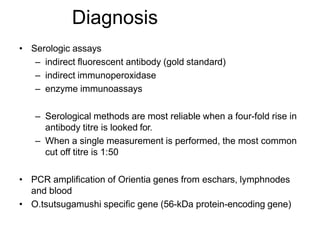
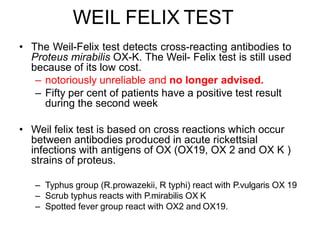
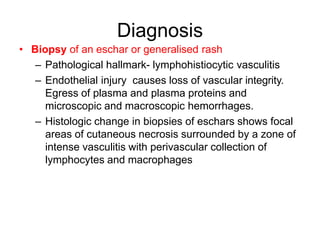
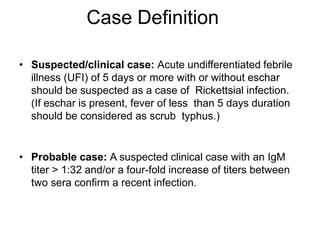
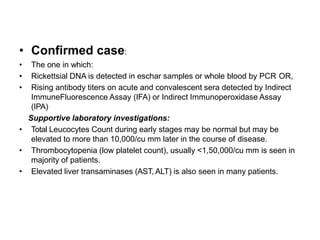
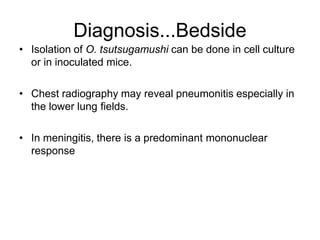
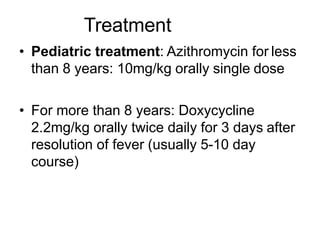
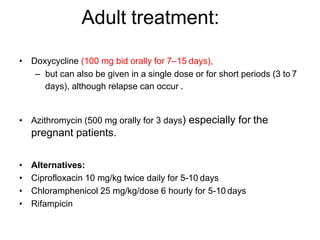
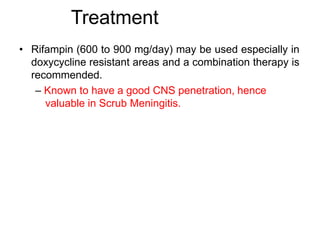
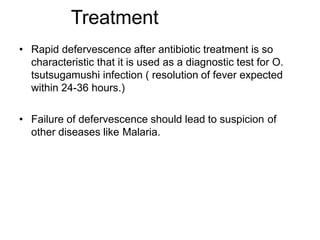
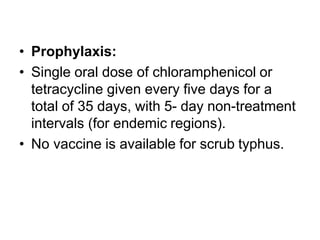
Scrub typhus is a mite-borne infectious disease caused by the bacteria Orientia tsutsugamushi. It is transmitted through the bites of larval trombiculid mites. The disease is characterized by high fever, headache, rash and commonly develops an eschar at the site of the mite bite. Complications can include pneumonia, acute respiratory distress syndrome, meningitis and multi-organ failure. Diagnosis is usually made through serologic testing like immunofluorescence assay, which detects IgM and IgG antibodies. Treatment involves doxycycline or azithromycin which is generally effective. Scrub typhus is endemic in parts of Asia and can cause fatalities if left untreated.