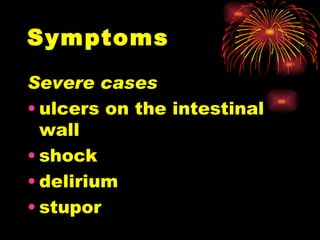
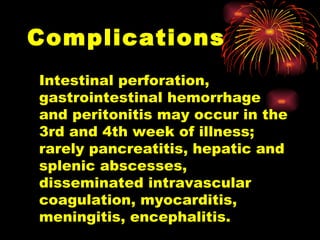
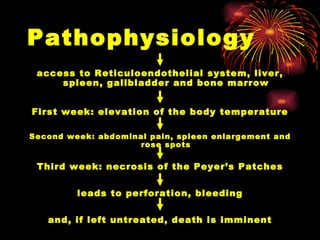
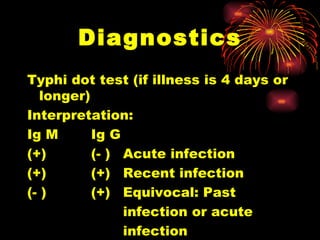
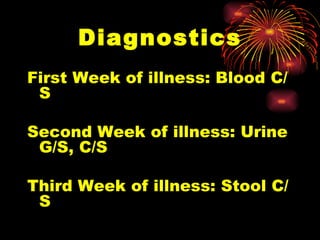
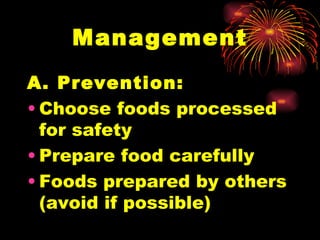
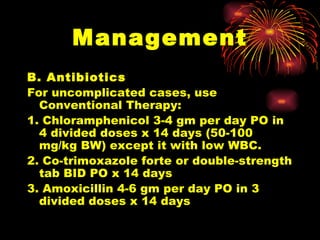
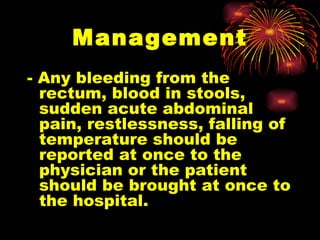
Typhoid Fever is caused by the bacterium Salmonella Typhi. It spreads through contaminated food or water and causes symptoms like sustained fever, abdominal pain, and headaches. Complications can include intestinal perforation or bleeding. Diagnosis involves blood or stool cultures. Treatment is with antibiotics like fluoroquinolones for 2 weeks. Prevention involves food and water safety as well as vaccination.








![Symptoms Fever [usually higher in the evening] - Intermittent Fever initially - Sustained Fever to high temperatures later](https://image.slidesharecdn.com/typhoid-fever-2-1234249024723946-2/85/Typhoid-Fever-10-320.jpg)