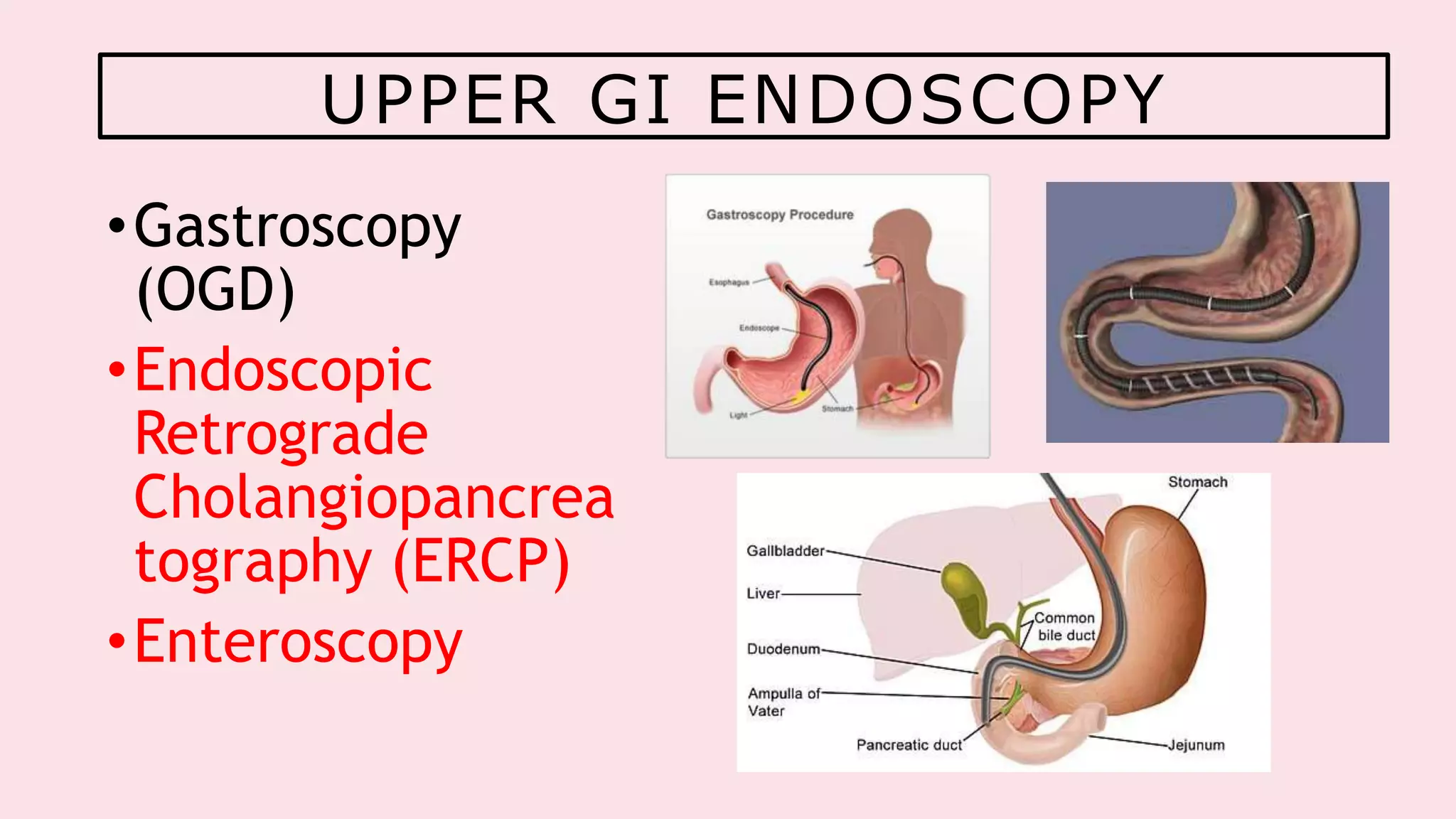
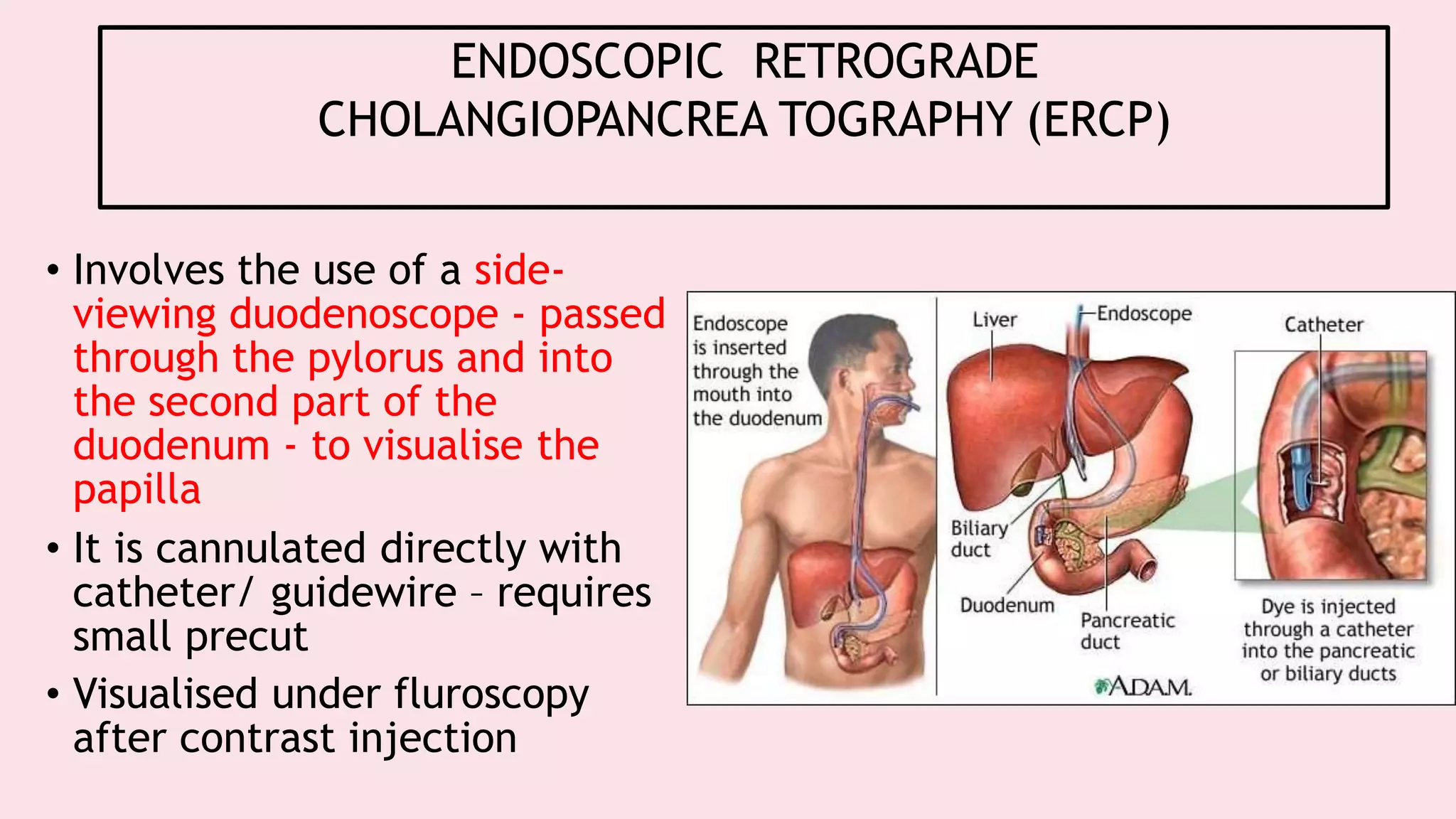
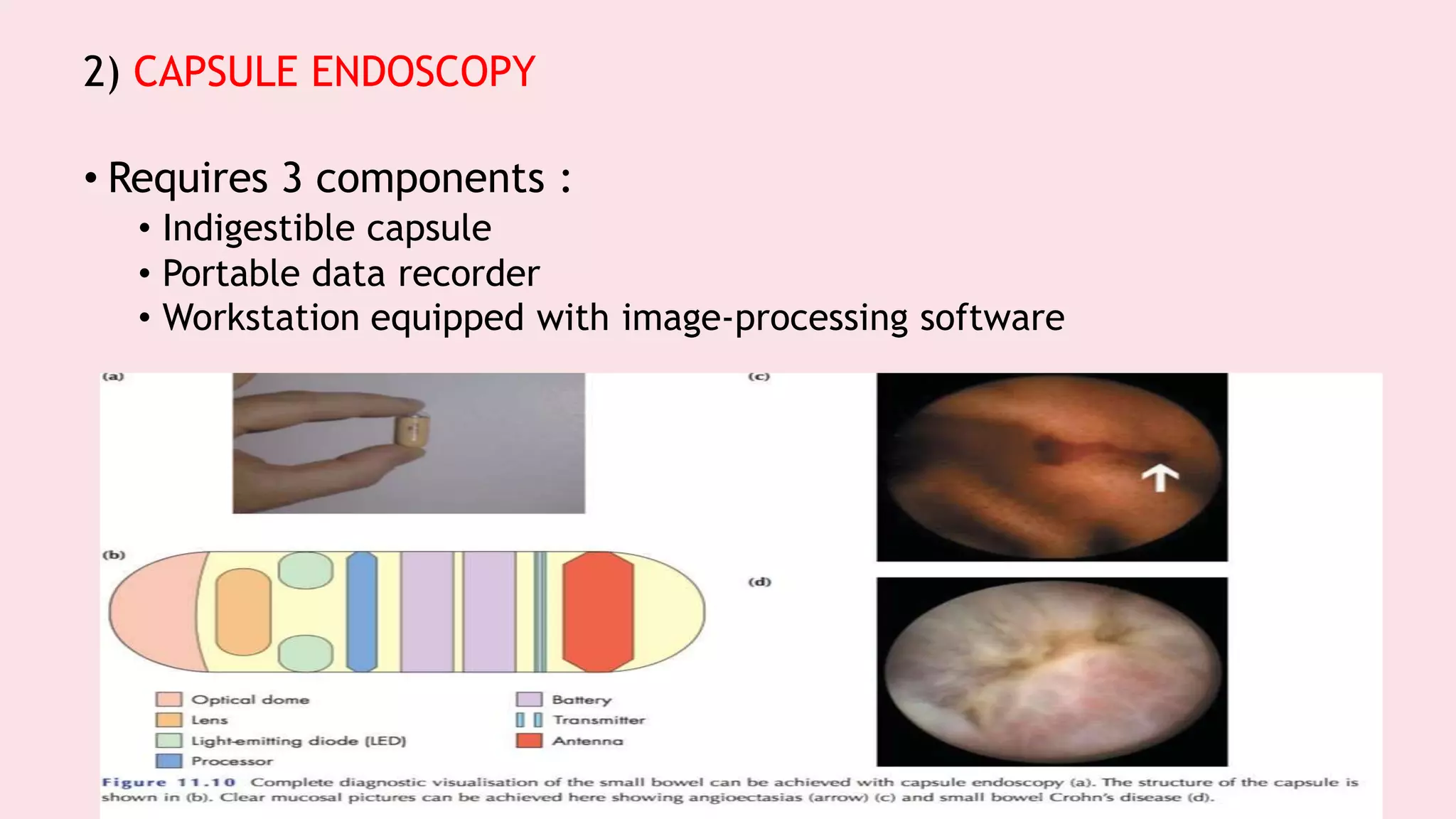
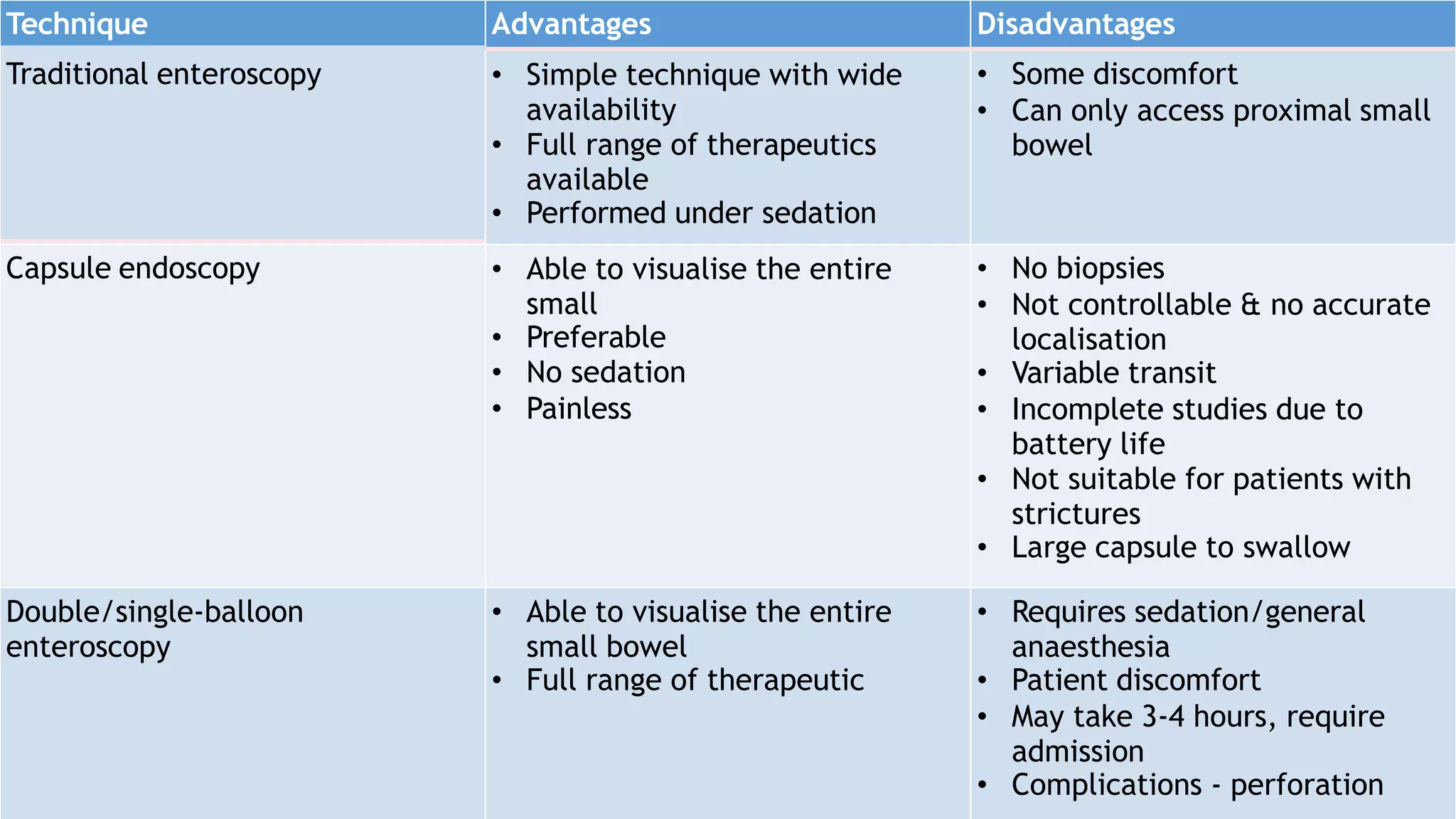
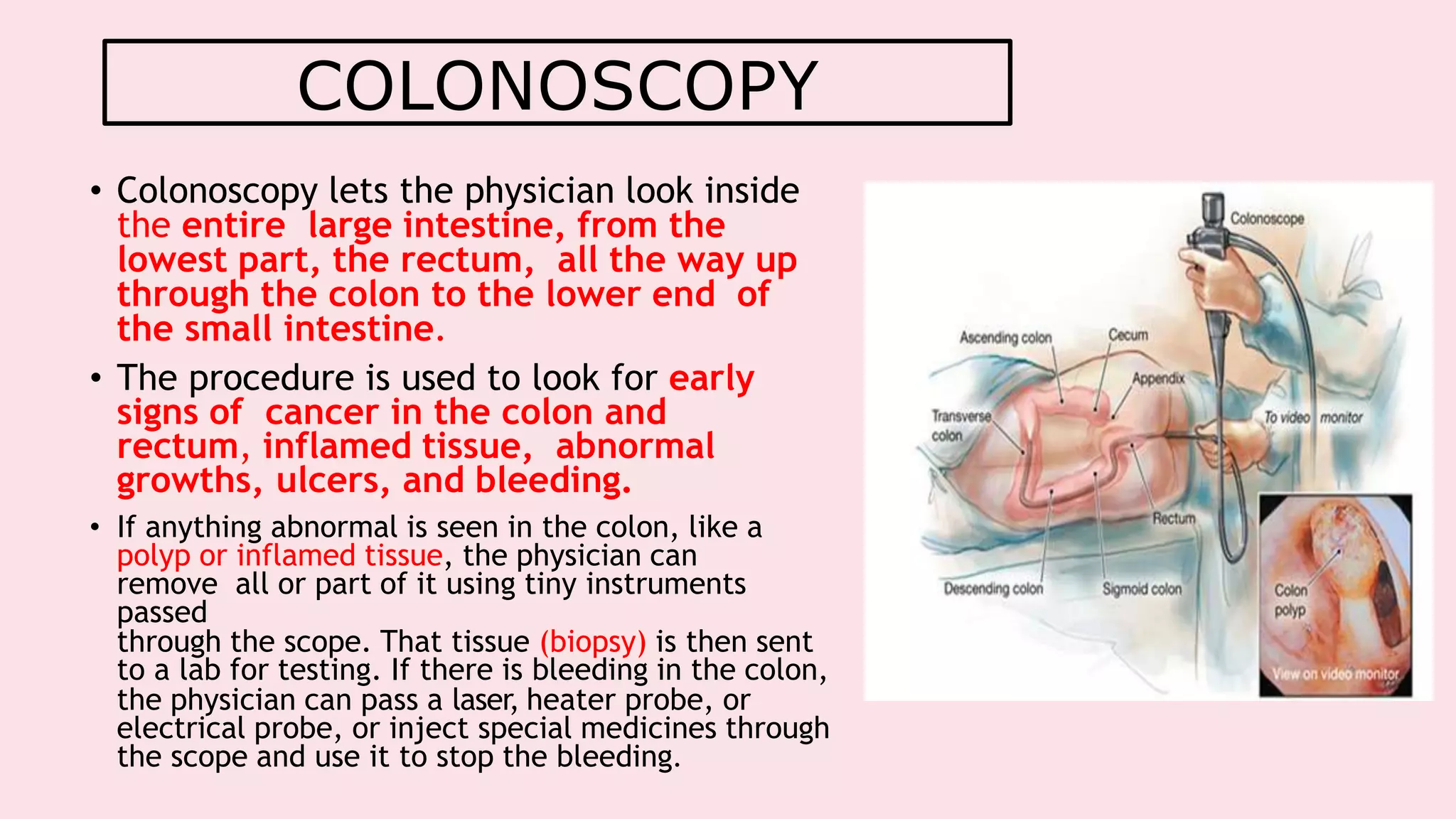
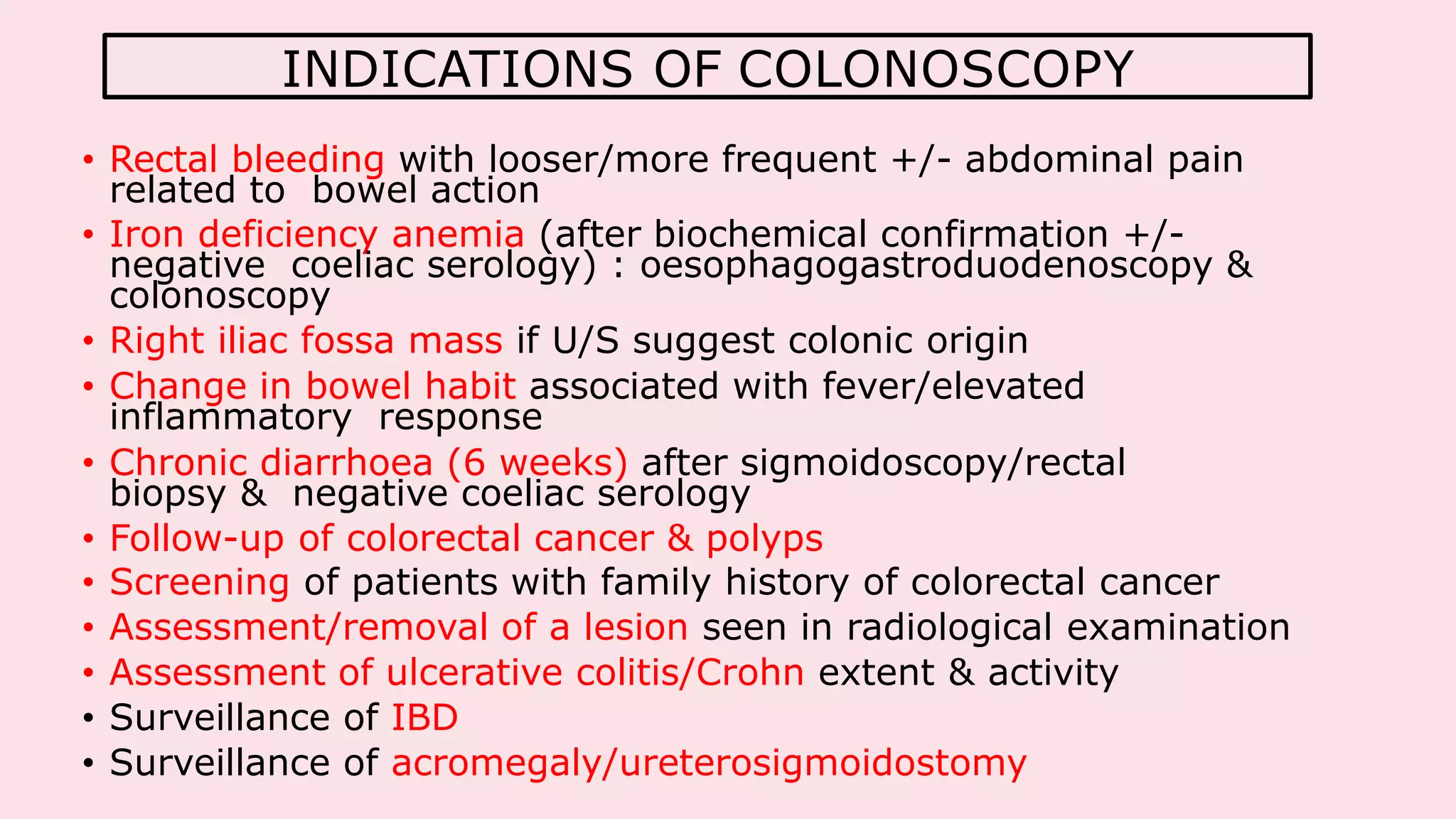
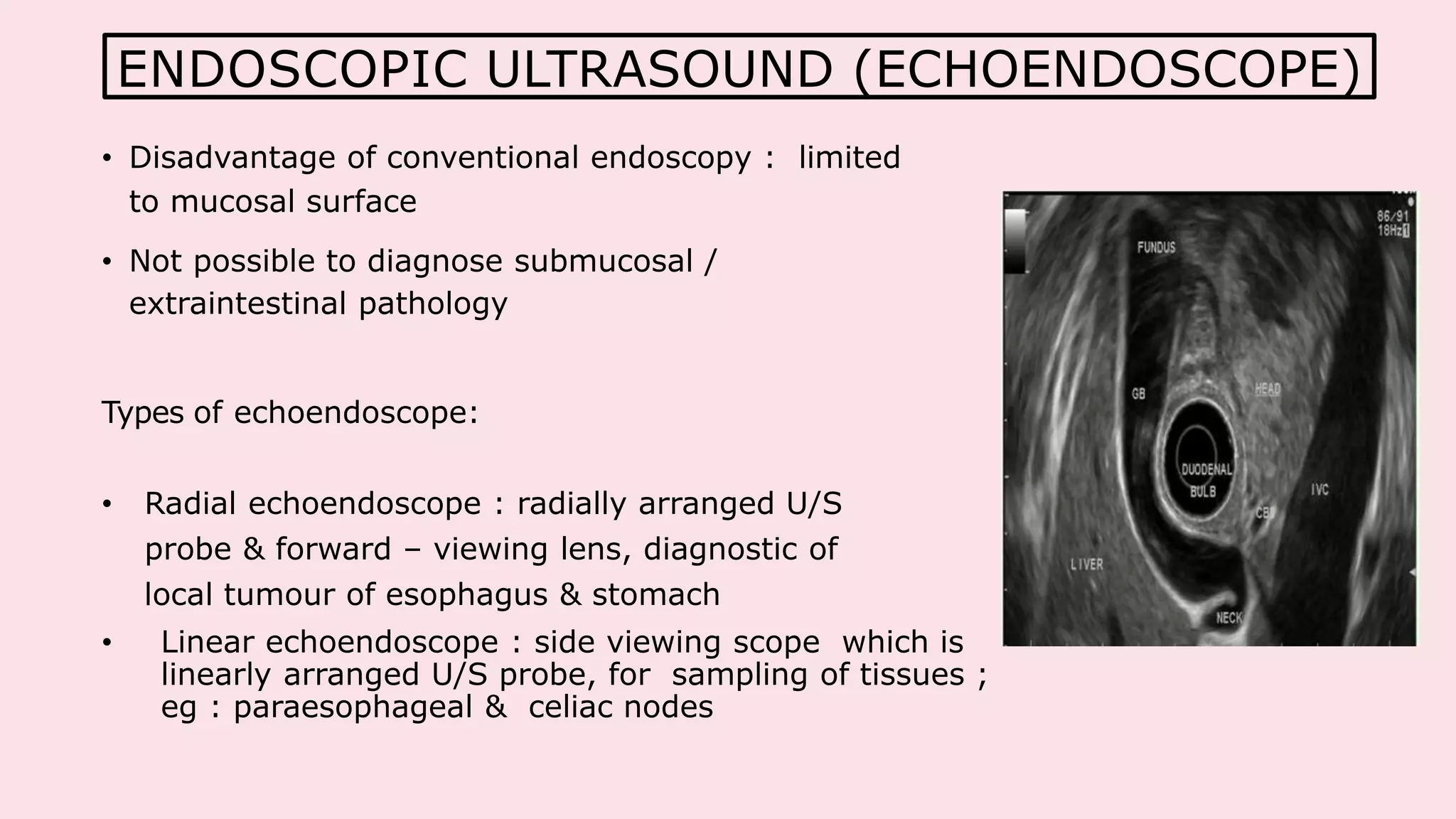
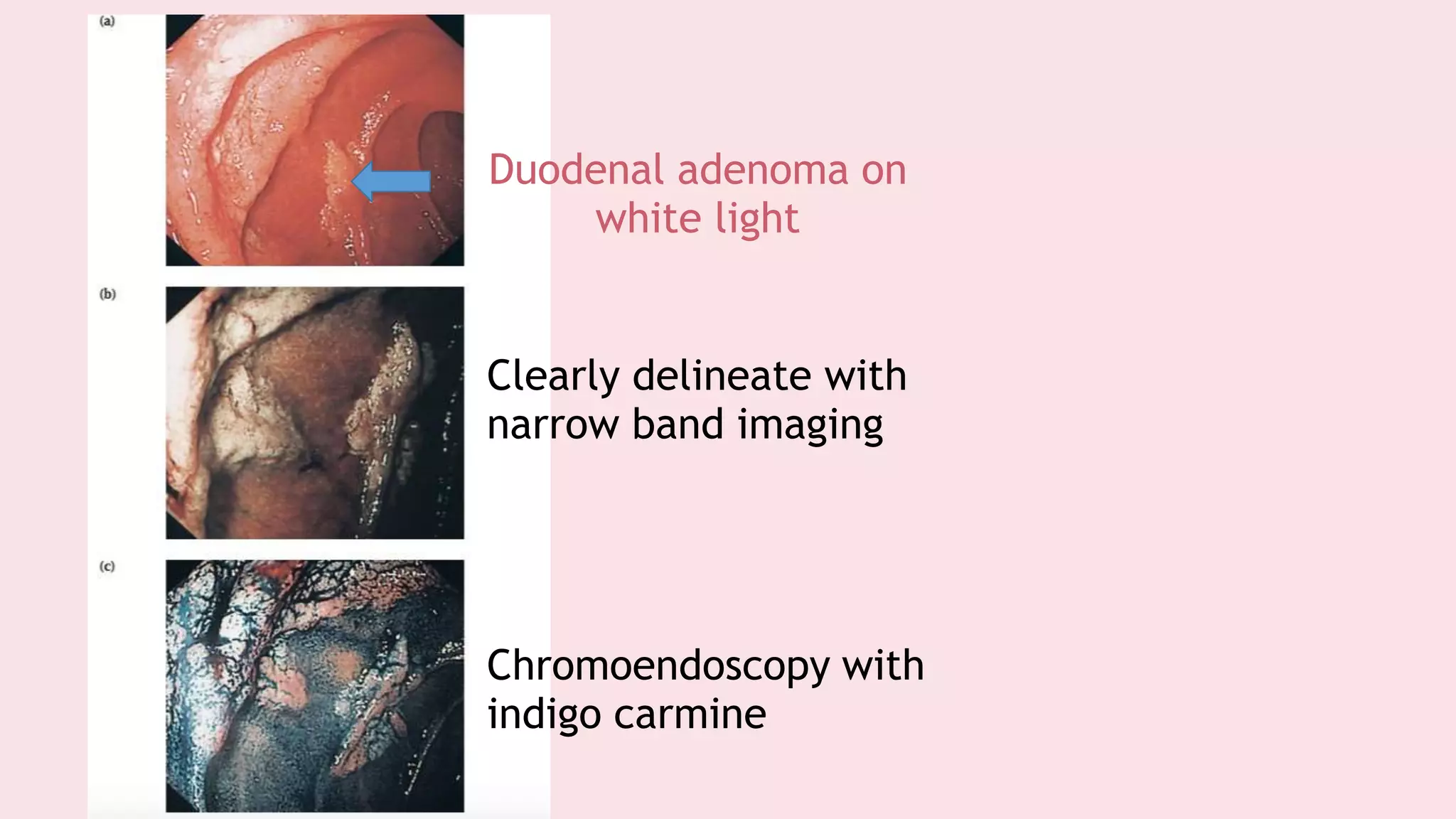
Endoscopy allows examination of body cavities using an endoscope. This document discusses various types of endoscopy including upper GI endoscopy (gastroscopy, ERCP), lower GI endoscopy (colonoscopy, sigmoidoscopy), and therapeutic endoscopy procedures. It describes the anatomy of the digestive tract, techniques, indications, and potential complications of different endoscopic procedures. New imaging technologies such as chromoendoscopy, narrow band imaging, and magnification endoscopy are also mentioned to improve tissue characterization during endoscopy.