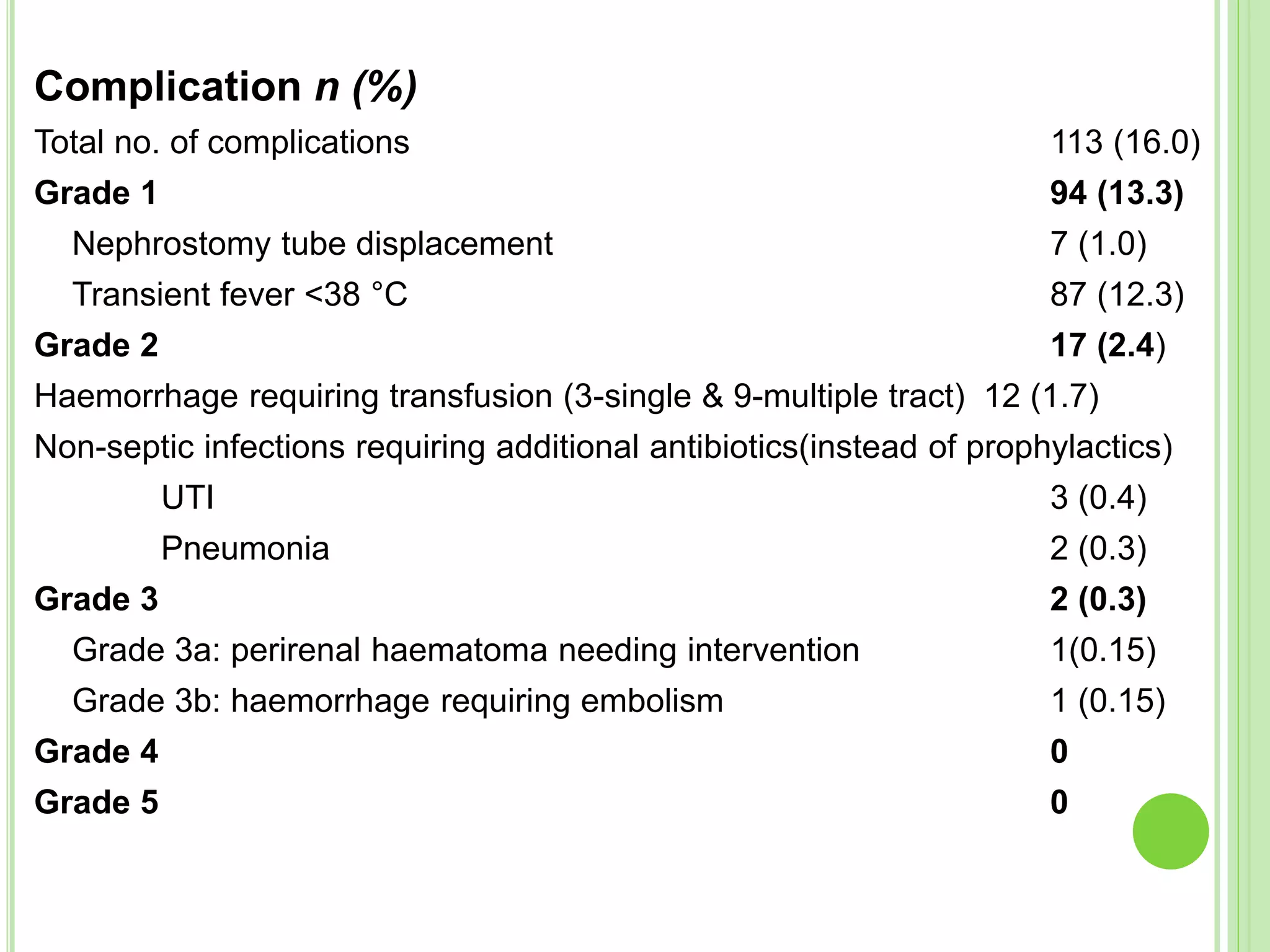
This study evaluated the safety and efficacy of percutaneous nephrolithotomy (PCNL) guided solely by ultrasonography in over 700 cases over 5 years. Access to the pelvicalyceal system was successful in all cases using ultrasonography. The overall stone-free rate was 87.4% and complications were minor, with a low 16% rate. The study demonstrated that PCNL can be performed safely and effectively using only ultrasonography guidance, avoiding the risks of radiation exposure from fluoroscopy.



![INTRODUCTION
Percutaneous nephrolithotomy (PCNL) has been
performed as a minimally invasive method of
removing kidney stones since 1976.
Because of the improvements in technique and
equipment, PCNL is now considered to be a
generally safe management option, with a low
incidence of complications [1,2]
1. Wen CC, Nakada SY. Treatment selection and outcomes: renal
calculi. Urol Clin North Am 2007; 34: 409–19
2. Lingeman JE, Miller NL. Management of kidney stones. BMJ
2007; 334: 468–72](https://image.slidesharecdn.com/pcnl-150819145642-lva1-app6891/75/Percutaneous-Nephrolithotomy-5-2048.jpg)
![ Pelvicalyceal system (PCS) access is key to
successful PCNL and is generally performed under
fluoroscopic guidance.
Although protective gowns can be used by patients
and physicians during these procedures, radiation
exposure can still affect the surgical team over the
long term, and the hazard is dose-independent [3].
3. Safak M, Olgar T, Bor D, Berkmen G, Gogus C. Radiation doses
of patients and urologists during percutaneous
nephrolithotomy. J Radiol Prot 2009; 29: 409–15](https://image.slidesharecdn.com/pcnl-150819145642-lva1-app6891/75/Percutaneous-Nephrolithotomy-6-2048.jpg)
![ The use of ultrasonography (US) can avoid
radiation exposure and provides a reliable method
for the localization of renal stones, especially non-
opaque stones that are not visible via fluoroscopy.
Moreover, colour US can be used as a tool for the
localization of intrarenal arteries and helps to avoid
their puncture by a Chiba needle [4,5].
4. Lu M-H, Pu X-Y, Gao X, Zhou X-F, Qiu J-G, Tu S-T. Comparative study of
clinical value of single B-mode ultrasound guidance and B-mode combined
with color Doppler ultrasound guidance in mini-invasive percutaneous
nephrolithotomy to decrease hemorrhagic complications. Urology 2010; 76:
815–20
5. Tzeng B-C, Wang C-J, Huang S-W, Chang C-H. Doppler ultrasound-guided
percutaneous nephrolithotomy: a prospective randomized study. Urology
2011; 78: 535–9](https://image.slidesharecdn.com/pcnl-150819145642-lva1-app6891/75/Percutaneous-Nephrolithotomy-7-2048.jpg)
![ Osman et al. [6] suggested that PCNL punctures should be
carried out under US guidance; however, they completed
the rest of the procedure under fluoroscopic guidance.
Some studies [7,8] have recommended the use of PCNL
guided solely by US for single stones in moderately to
markedly dilated PCSs by an experienced urologist
6. Osman M, Wendt-Nordahl G, Heger K, Michel MS, Alken P, Knoll T.
Percutaneous nephrolithotomy with ultrasonography- guided renal access:
experience from over 300 cases. BJU Int 2005; 96: 875–8
7. Hosseini M, Hassanpour A, Farzan R, Yousefi A, Afrasiabi MA.
Ultrasonography guided percutaneous nephrolithotomy. J Endourol 2009;
23: 603–7
8. Gamal WM, Hussein M, Aldahshoury M, Hammady A, Osman M, Moursy E,
Abuzeid A. Solo ultrasonography-guided percutanous nephrolithotomy for
single stone pelvis. J Endourol 2011; 25: 593–6](https://image.slidesharecdn.com/pcnl-150819145642-lva1-app6891/75/Percutaneous-Nephrolithotomy-8-2048.jpg)
![ Mayank et al. [9] suggested US as an adjunct to
fluoroscopy for renal access in PCNL; however, a
large series is still needed to prove the safety and
efficiency of PCNL guided solely by US in various
stone cases. In the present study, we reported our
experience and evaluated the feasibility and
efficacy of PCNL performed solely under US
guidance.
9. Agarwal M, Agrawal MS, Jaiswal A, Kumar D, Yadav H, Lavania P. Safety
and efficacy of ultrasonography as an adjunct to fluoroscopy for renal
access in percutaneous nephrolithotomy (PCNL). BJU Int 2011; 108:
1346–9](https://image.slidesharecdn.com/pcnl-150819145642-lva1-app6891/75/Percutaneous-Nephrolithotomy-9-2048.jpg)
![PATIENTS AND METHODS
From May 2007 to July 2012, 705 24-F-tract PCNL
procedures were performed (679 patients, of whom
26 had bilateral stones).
Calyceal puncture and dilatation were performed
under US guidance in all cases.
The procedure was evaluated for access success,
length of postoperative hospital stay, complications
(modified Clavien system) [10], stone clearance
and the need for auxiliary treatments.
10. de la Rosette JJ, Opondo D, Daels FP et al. Categorisation of
complications and validation of the Clavien score for
percutaneous nephrolithotomy. Eur Urol 2012; 62: 246–55](https://image.slidesharecdn.com/pcnl-150819145642-lva1-app6891/75/Percutaneous-Nephrolithotomy-10-2048.jpg)










![DISCUSSION
Percutaneous nephrolithotomy is the primary procedure
for the management of patients with renal stones who
are not candidates for ESWL.
Fluoroscopic guidance has been used to guide the
percutaneous renal access, establish the working tract
and perform the stone manipulation.
The use of US guidance has other advantages in
addition to being free of ionizing radiation; for example,
it results in fewer punctures, has shorter operating times
and avoids contrast-related complications [12].
12. Basiri A, Ziaee SA, Nasseh H et al. Totally ultrasonography guided
percutaneous nephrolithotomy in the flank position. J Endourol 2008;
22: 1453–7](https://image.slidesharecdn.com/pcnl-150819145642-lva1-app6891/75/Percutaneous-Nephrolithotomy-27-2048.jpg)
![ This form of guidance allows imaging of the intervening
structures with the benefit of minimizing the risk of injury
to nearby organs.
Moreover, the use of US at the end of the procedure
helps the urologist to look for non-opaque and semi-
opaque residual stones that are not visualized by
radiography [13].
The European Association of Urology recommends
initial puncture under US guidance because it reduces
radiation hazards [14].
13. Basiri A, Ziaee A, Kianian H, Mehrabi S, Karami H, Moghaddam S.
Ultrasonographic versus Fluoroscopic Access for Percutaneous
Nephrolithotomy: a Randomized Clinical Trial. J Endourol 2008; 22: 281-
4
14. European Association of Urology. Guidelines on urolithiasis. 2012
http://www.uroweb.org/gls/pdf/21_Urolithiasis_LR.pdf](https://image.slidesharecdn.com/pcnl-150819145642-lva1-app6891/75/Percutaneous-Nephrolithotomy-28-2048.jpg)

![ 100% access to the kidney as well as 87.4% complete
stone clearance, were achieved. The stone-free rate in
this series was comparable with the rates gained from
PCNL results reported in other series under either US or
fluoroscopic guidance [15,16].
Osman et al. [17] reported that the sensitivity of plain
abdominal film of kidney, ureter and bladder (KUB) for
detecting stone-free rates was 40.3% and that of US
was 37.1%.
15. Shoma AM, Eraky I, El-Kenawy M, El-Kappany HA. Percutaneous
nephrolithotomy in the supine position: technical aspects and
functional outcome compared with the prone technique. Urology 2002;
60: 388–92
16. Basiri A, Mohammadi Sichani M, Hosseini SR et al. X-ray-free
percutaneous nephrolithotomy in supine position with ultrasound
guidance.World J Urol 2010; 28: 239–44
17. Osman Y, El-Tabey N, Refai H et al. Detection of residual stones
after percutaneous nephrolithotomy: role of non-enhanced spiral
computerized tomography. J Urol 2008; 179: 198–200](https://image.slidesharecdn.com/pcnl-150819145642-lva1-app6891/75/Percutaneous-Nephrolithotomy-30-2048.jpg)
![ The sensitivities of KUB and US for detecting significant
residual stones were reported to be 58.3 and 41.6%,
respectively; for detecting CIRFs, the reported
sensitivities were 15.3 and 30.7%, respectively;
however, Alan et al. [18] reported that the sensitivities of
US for detecting significant residual stones and CIRFs
were 83.3 and 87.5%, respectively, based on KUB
detection.
In their study, the stone-free status was double-checked
during the operation using a flexible nephroscope and
US, but CT was also routinely performed to confirm the
residual stone status on the second postoperative day.
18. Alan C, Kocoğlu H, Ates F, Ersay AR. Ultrasound-guided X-ray free
percutaneous nephrolithotomy for treatment of simple stones in the
flank position. Urol Res 2011; 39: 205–12](https://image.slidesharecdn.com/pcnl-150819145642-lva1-app6891/75/Percutaneous-Nephrolithotomy-31-2048.jpg)
![ Percutaneous nephrolithotomy is usually performed with the
patient in a prone position, but this prone position has several
disadvantages. For example, PCNL with the patient in this
position is difficult when the patient is obese or has spinal
anomalies or cardiovascular disease [19].
Karami et al. [20] reported performing PCNL under US guidance
in 40 patients in the lateral position with an access rate of 100%
and a complete stone-removal rate of 85%.
In the present study, PCNL was performed in the lateral position
for the 53 patients who had insufficient cardiac output or
pulmonary disease and US guidance was proven to be a safe
and convenient procedure in both positions.
19. Manohar T, Jain P, Desai M. Supine percutaneous nephrolithotomy: effective approach
to high-risk and morbidly obese patients. J Endourol 2007; 21: 44–9
20. Karami H, Arbab AH, Rezaei A, Mohammadhoseini M, Rezaei I. Percutaneous
nephrolithotomy with ultrasonography-guided renal access in the lateral decubitus
flank position. J Endourol 2009; 23: 33–5](https://image.slidesharecdn.com/pcnl-150819145642-lva1-app6891/75/Percutaneous-Nephrolithotomy-32-2048.jpg)