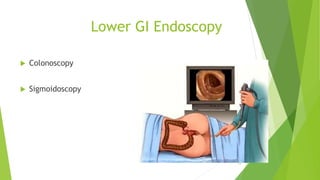
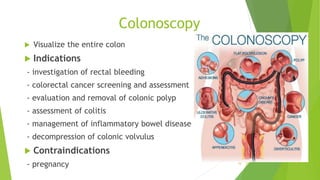
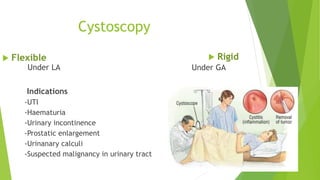
The document provides an overview of endoscopy in clinical surgery, detailing its uses for investigation, diagnosis, therapy, and monitoring of various conditions within the gastrointestinal, urinary, respiratory, and reproductive systems. It outlines specific types of endoscopic procedures, patient preparation, potential complications, and the necessity of informed consent. Additionally, it highlights the equipment used, classifications, and procedural guidelines essential for successful endoscopic interventions.