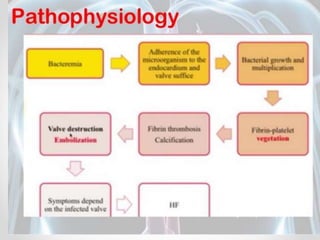
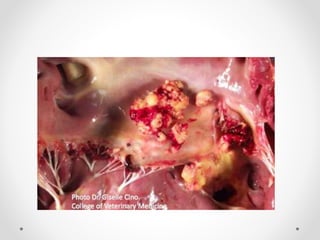
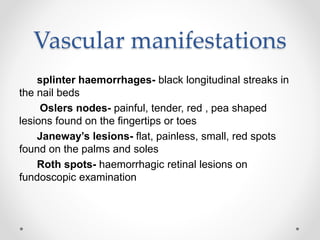
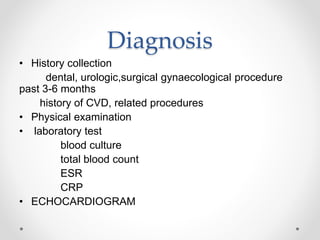
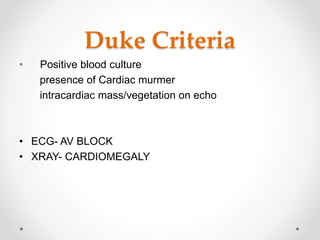
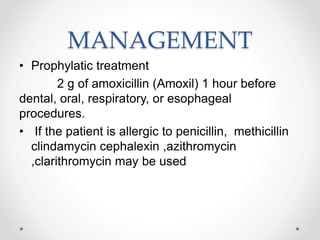
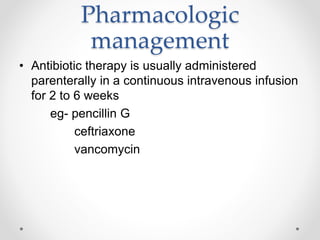
Endocarditis is an inflammation of the inner layer of the heart. There are two main types: infective and non-infective. Infective endocarditis involves the heart valves and is caused most commonly by bacteria or fungi in people with preexisting heart conditions. It can develop suddenly (acute) or slowly (subacute) and symptoms may include fever, weakness, and heart murmurs. Diagnosis involves blood cultures, echocardiogram, and applying the Duke Criteria. Treatment consists of intravenous antibiotics for several weeks along with possible valve replacement surgery if valves are severely damaged.