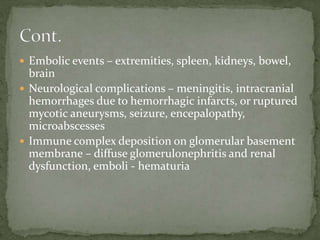
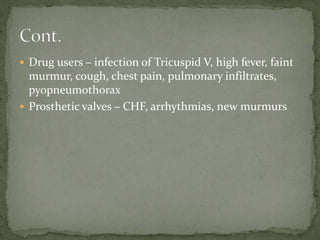
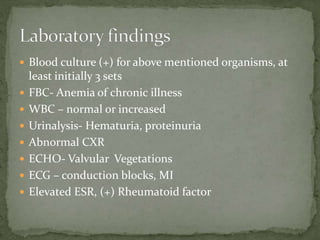
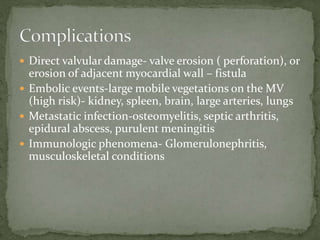
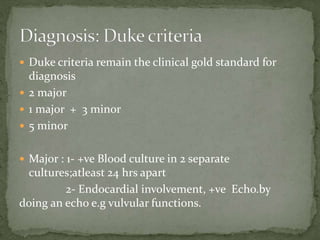
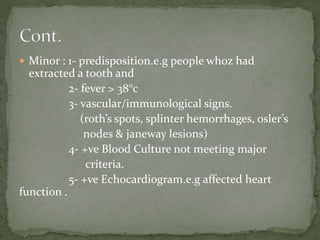
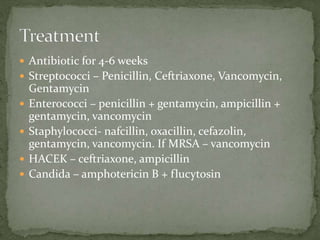
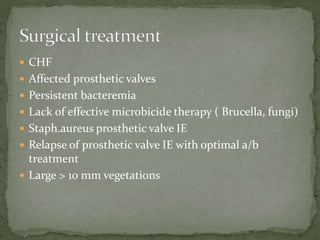
The document discusses infective endocarditis, a bacterial infection of the heart's endocardial surface that often leads to severe complications. It covers the causative organisms, risk factors, symptoms, diagnostic criteria, and treatment options, emphasizing the need for early detection and management. The Duke criteria are highlighted as the standard for diagnosis, with various antibiotics recommended based on the pathogen involved.