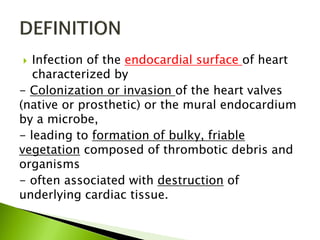
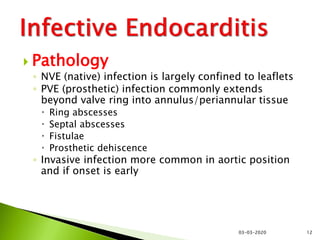
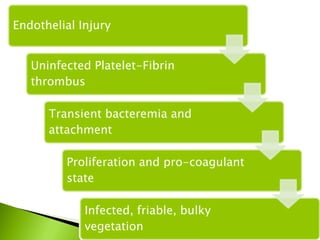
The document discusses infective endocarditis, which is an infection of the inner lining of the heart chambers and heart valves. It describes the types of infective endocarditis as native valve, prosthetic valve, or intravenous drug abuser infective endocarditis. It covers the typical causative organisms, pathophysiology, clinical manifestations, diagnosis and treatment of this condition.