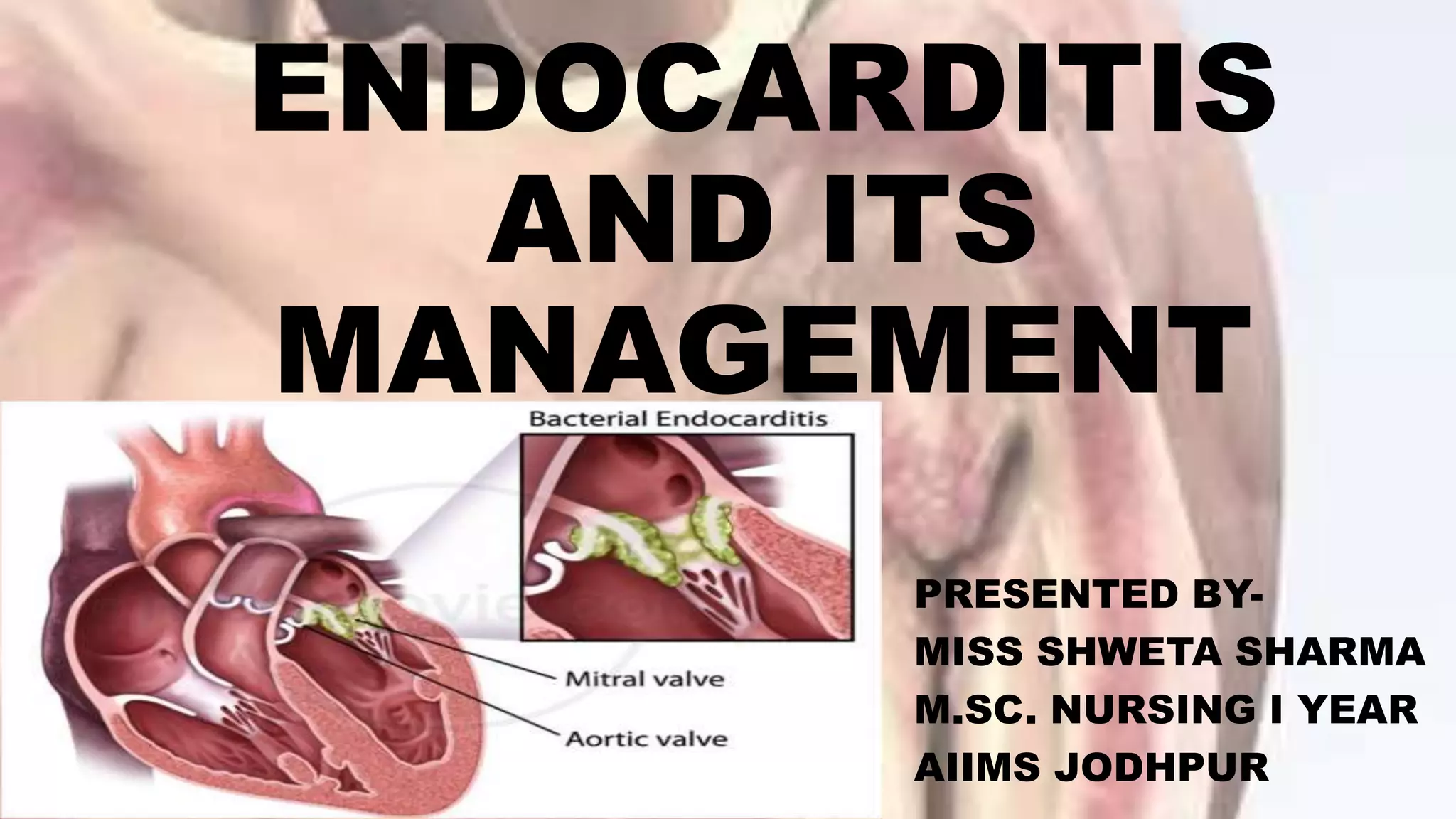
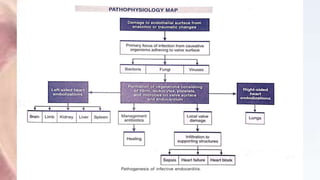
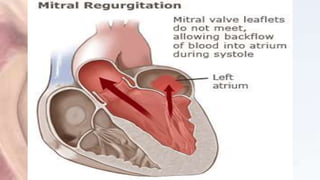
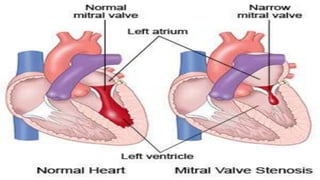
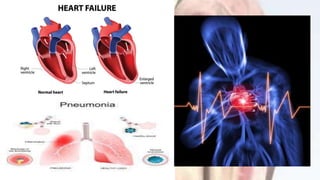
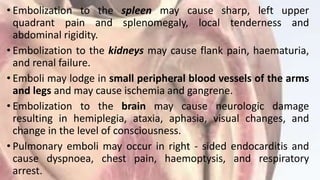
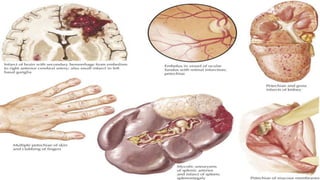
This document provides information about infective endocarditis, including its causes, risk factors, clinical manifestations, diagnosis, treatment, nursing care, and prevention. Infective endocarditis is an infection of the heart valves and lining that can be caused by bacteria or fungi entering the bloodstream. It requires long-term antibiotic treatment and may necessitate valve replacement surgery if complications occur. Nurses monitor for symptoms, assess treatment effectiveness, and educate patients on preventing future infections.
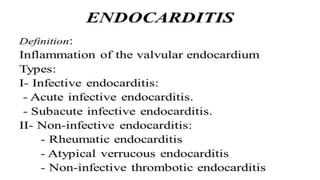
![Classification of infective endocarditis:
•Acute form - Affects those with healthy valves and
manifests as a rapidly progressive illness.
•Subacute form – Affects those with pre-existing valve
disease and has a clinical course that may extend over
months.
•Infective endocarditis can also be classified based on
the cause (e.g., IV drug abuse IE, fungal endocarditis)
or site of involvement (e.g., prosthetic valve
endocarditis [PVE]).](https://image.slidesharecdn.com/endocarditis-200605111621/85/Endocarditis-and-its-management-5-320.jpg)




![REFERENCES
• 1. Janice L. Hinkle, Kerry H. Cheever. Brunner and Suddarth’s Textbook of Medical
Surgical Nursing. 2015. New Delhi. Wolters Kluwer.13th Edition. Volume 2. Pg. no. 780-
782.
• 2. Lewis. Medical Surgical Nursing Assessment and Management of clinical
problems.2015. New Delhi. Elsevier. 2nd Edition. Volume I. Pg. no. 847-851.
• 3. PubMed. Clinic microbiological spectrum of infective endocarditis - from a tertiary care
centre in south India. Iran J Microbiol. 2017 Oct; 9(5): 257–263. Available from
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5748443/ [cited 11 April 2020]
• 4. PubMed. In-hospital infective endocarditis following transcatheter aortic valve
replacement: a cross-sectional study of the National Inpatient Sample database in the
USA. J Hosp Infect. 2018 Dec;100(4):444-450. doi: 10.1016/j.jhin.2018.05.014. Epub 2018
May 25. Available from https://www.ncbi.nlm.nih.gov/pubmed/29803809 [cited 11 April
2020]
• 5. PubMed. Relationship of oral conditions to the incidence of infective endocarditis in
periodontitis patients with valvular heart disease: a cross-sectional study. Clin Oral
Investig. 2020 Feb;24(2):833-840. doi: 10.1007/s00784-019-02973-2. Epub 2019 Jun 13.
Available from https://www.ncbi.nlm.nih.gov/pubmed/31197658 [cited 11 April 2020]](https://image.slidesharecdn.com/endocarditis-200605111621/85/Endocarditis-and-its-management-42-320.jpg)

