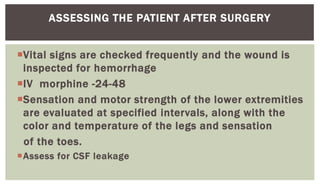
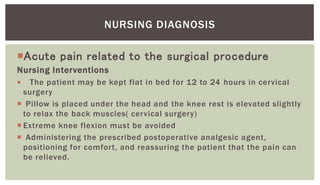
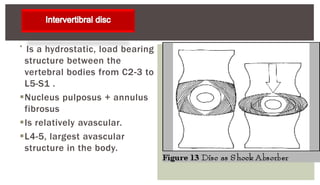
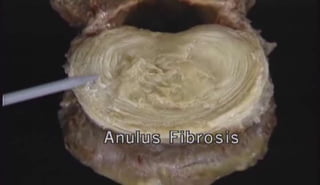
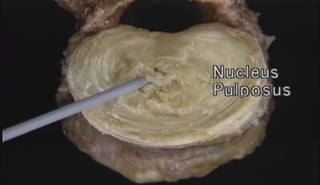
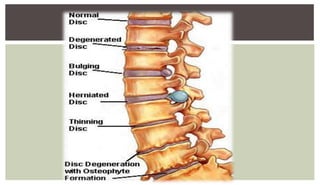
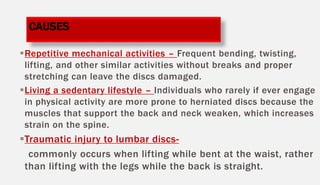
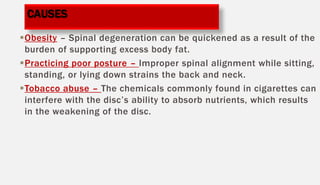
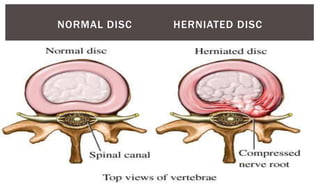
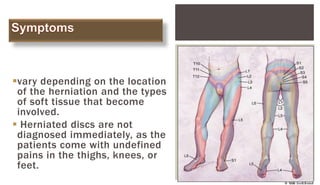
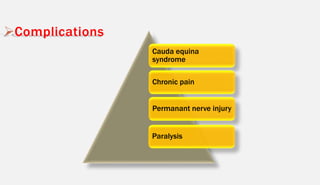
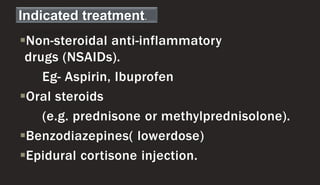
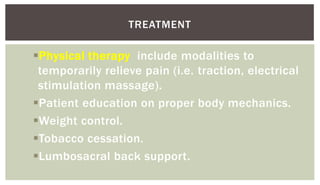
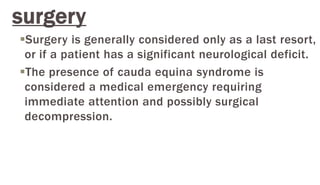
An intervertebral disc prolapse occurs when a tear in the outer ring of an intervertebral disc allows the inner nucleus pulposus to bulge out. The document discusses the anatomy and functions of intervertebral discs, causes and types of disc prolapses, symptoms, diagnostic tests, treatment options including medications, physical therapy, injections, and various surgical procedures. Nursing care focuses on preoperative teaching, postoperative monitoring for complications, managing pain, and providing education on mobility restrictions and home care.






![CHEMONUCLEOLYSIS-
Chemonucleolysis is the term
used to denote chemical
destruction of nucleus pulposus
[Chemo+nucleo+lysis].
This involves intradiscal
injection of
chymopapain which causes
hydrolysis of he cementing
protein of the nucleus pulposus.
This causes decrease in water
binding capacity leading to
reduction in size and drying the
disc.](https://image.slidesharecdn.com/intervertebraldiscprolapseivdp-171013100709/85/Intervertebral-disc-prolapse-ivdp-31-320.jpg)