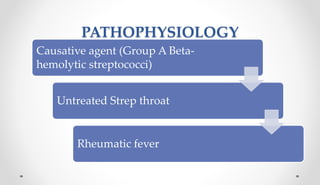
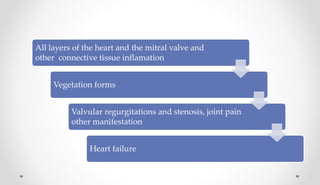
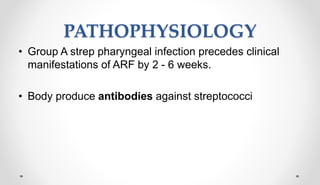
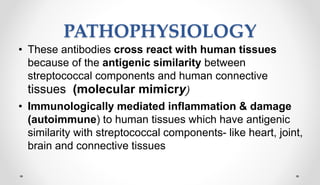
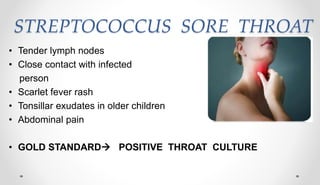
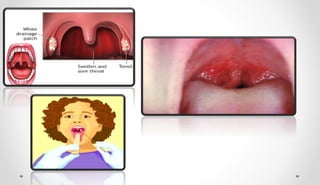
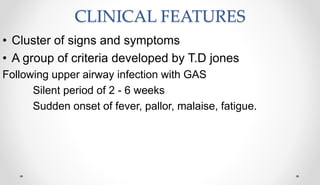
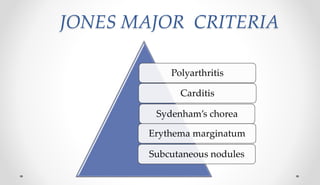
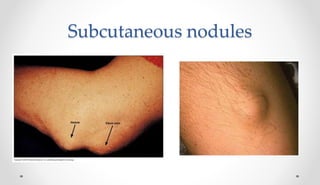
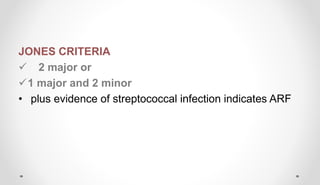
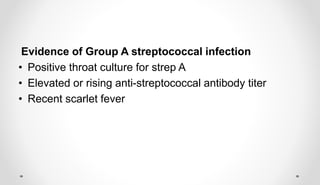
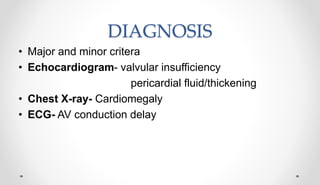
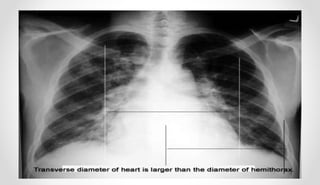
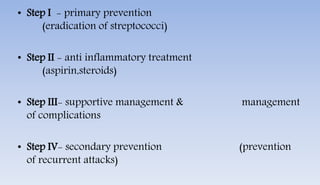
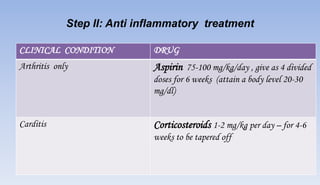
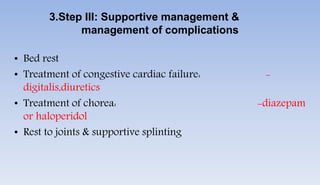
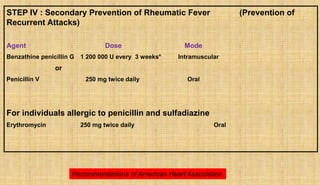
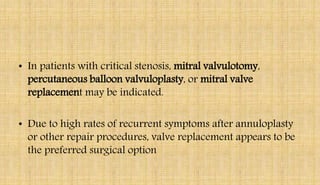
Rheumatic fever and heart disease are caused by an autoimmune reaction to a Group A streptococcal infection. Acute rheumatic fever causes inflammation of the heart and valves, which can lead to rheumatic heart disease characterized by scarring and deformity of the heart valves. Symptoms include polyarthritis, carditis, chorea, and subcutaneous nodules. Treatment involves bed rest, anti-inflammatory drugs, antibiotics to prevent recurrence, and possible heart valve surgery for complications like stenosis. Nursing care focuses on managing pain, cardiac output, and ensuring patient education about the chronic nature of rheumatic heart disease.