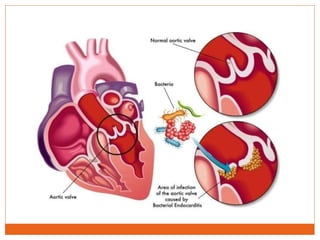
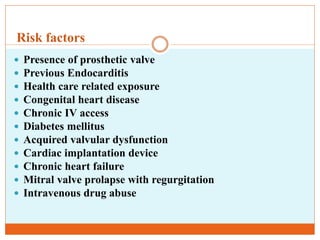
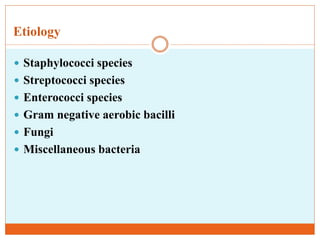
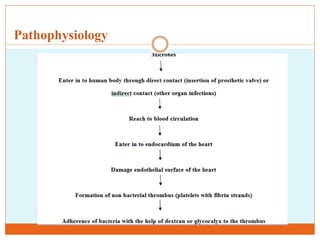
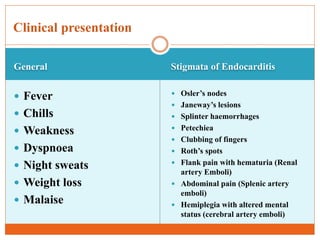
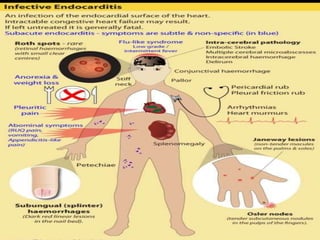
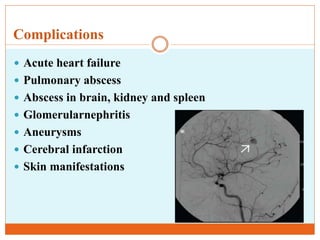
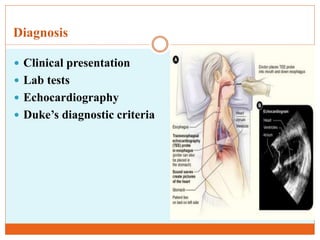
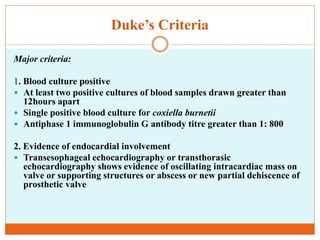
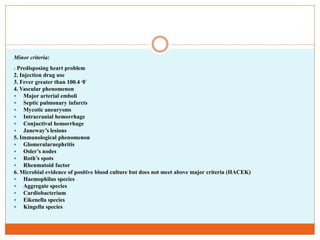
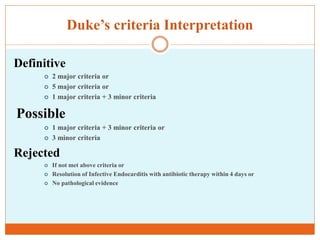
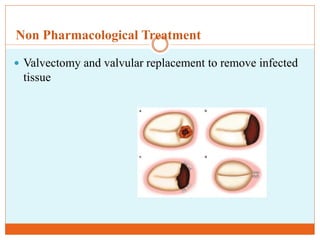
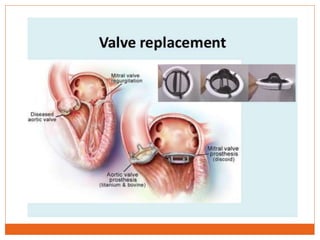
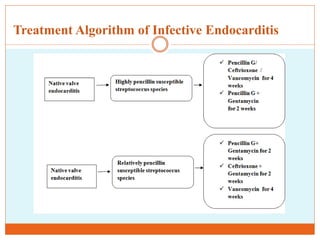
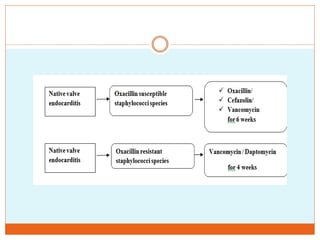
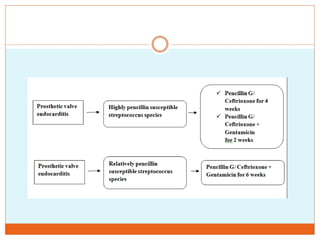
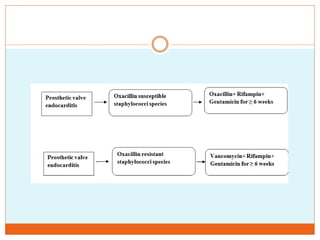
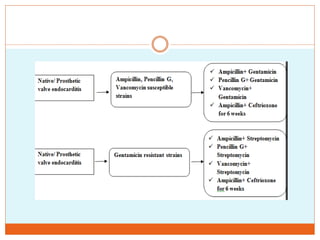
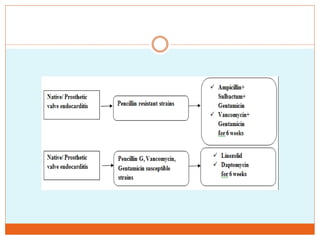
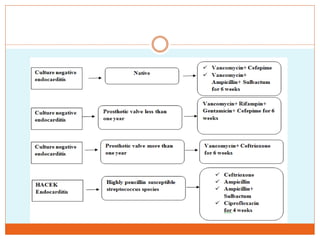
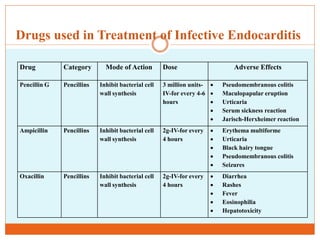
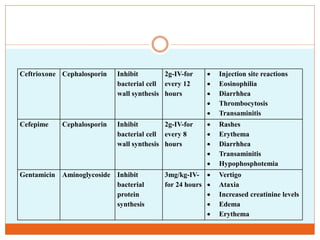
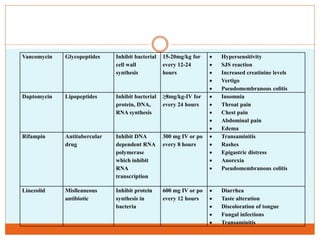
The document defines infective endocarditis as an inflammation of the inner lining of the heart chambers and heart valves, most commonly caused by bacterial infections. It affects 3-7.5 people per 100,000 worldwide each year. Common causes are streptococcus species in India and staphylococcus aureus in acute cases. Risk factors include prosthetic heart valves, IV drug use, and congenital heart defects. Treatment involves antibiotics to kill the infecting bacteria as well as potential heart valve replacement surgery if the infection damages heart valves.