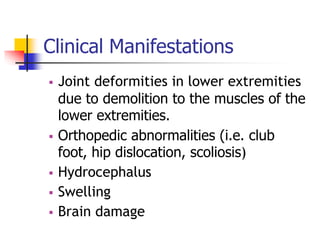
The document discusses Spinal Bifida, beginning with the group members presenting and objectives of the presentation. It defines Spinal Bifida as a birth defect involving failure of vertebral arch fusion. It describes the types (Occulta, Cystica with Meningocele and Myelomeningocele forms) and discusses etiology, pathophysiology, clinical manifestations, diagnostic tests, medical and nursing management, and complications of Spinal Bifida. The presentation aims to provide knowledge on Spinal Bifida and its characteristics to students.