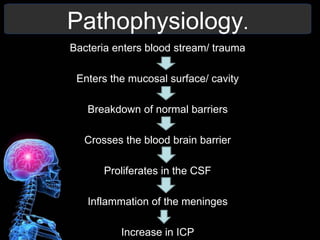
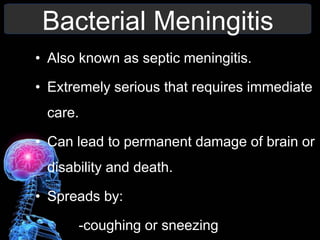
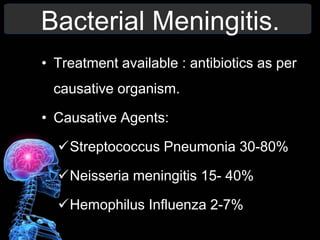
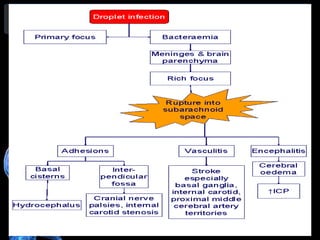
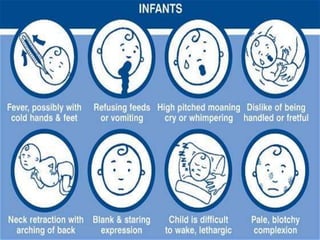
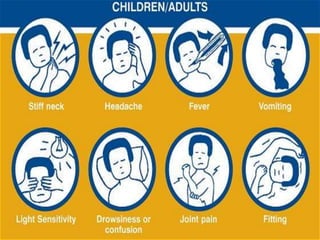
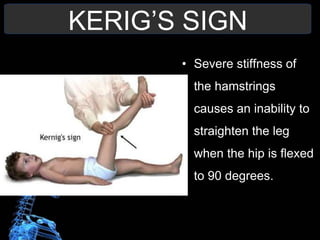
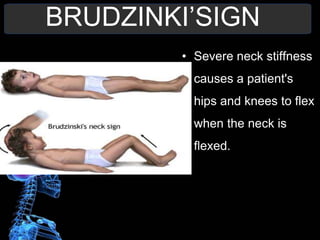
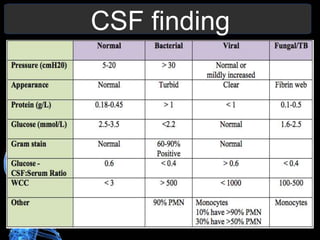
A 15-year-old male with leukemia was admitted with symptoms of disturbed gait, fever, vomiting, headache, and drowsiness. He also had nuchal rigidity and photophobia. These symptoms suggest a diagnosis of meningitis. Key aspects of managing meningitis include administering antibiotics based on the causative organism, monitoring for complications like seizures and impaired cognition, and providing supportive care. Nursing priorities involve assessing respiratory function, managing pain and mobility issues, ensuring adequate nutrition, and addressing patient anxiety. Lumbar puncture and CSF examination are important for confirming a diagnosis of bacterial meningitis.