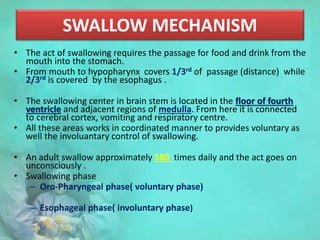
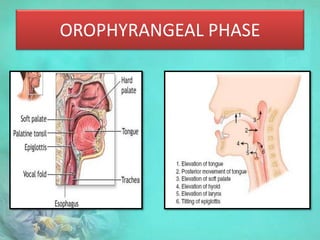
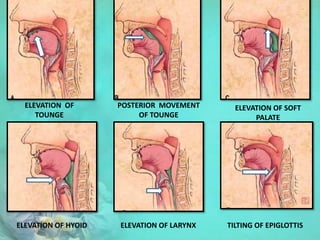
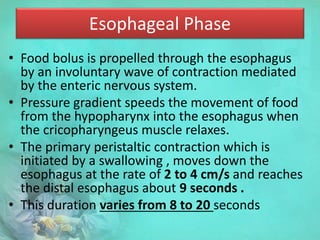
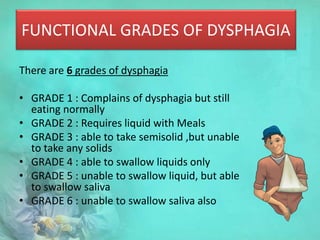
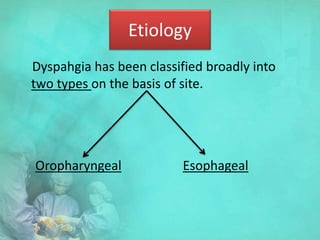
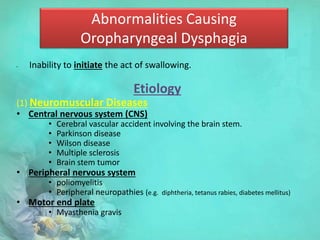
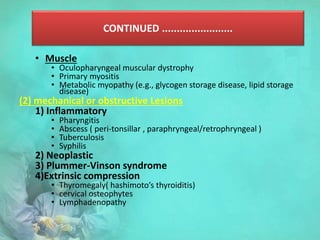
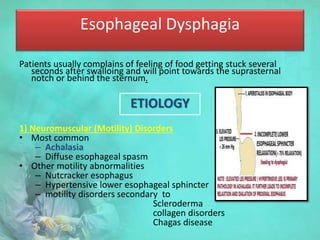
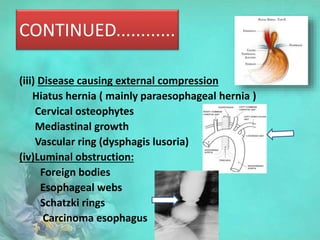
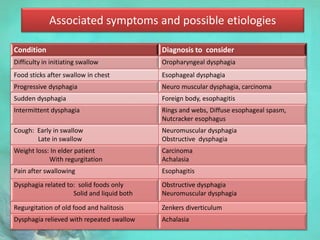
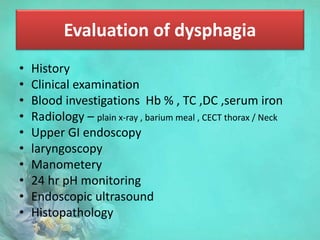
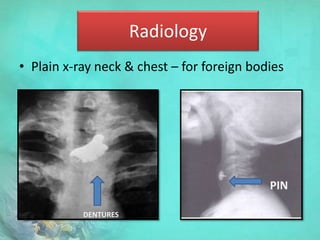
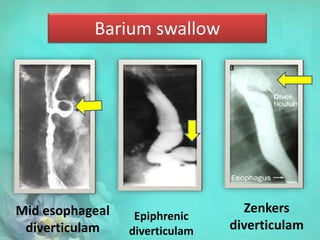
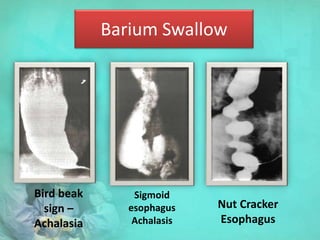
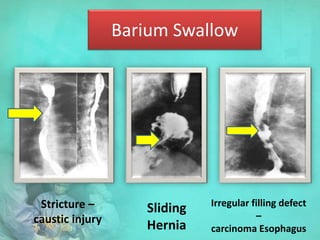
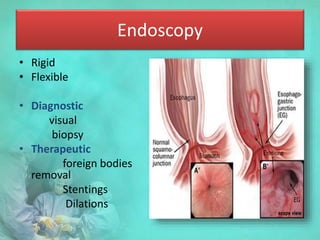
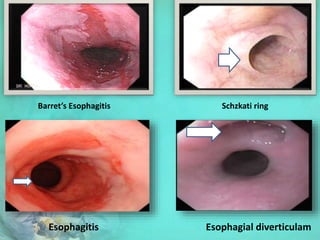
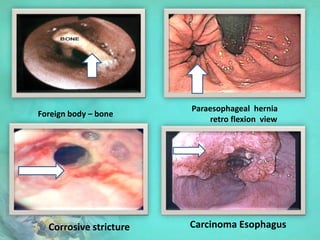
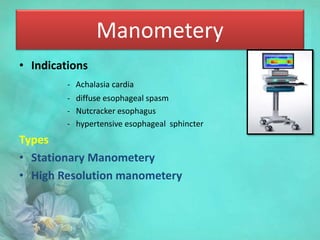
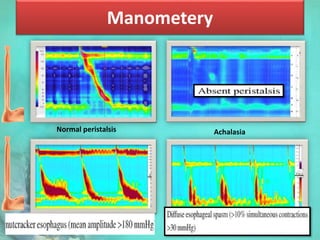
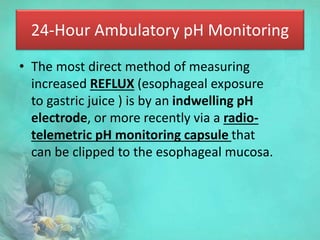
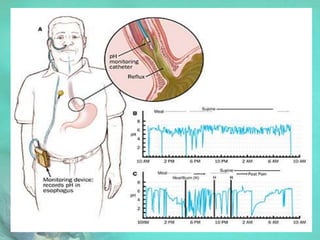
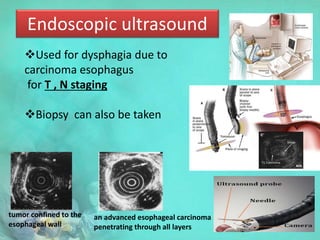
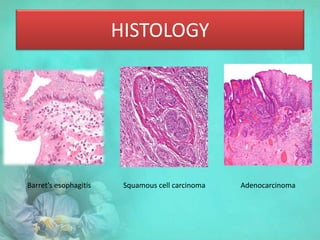
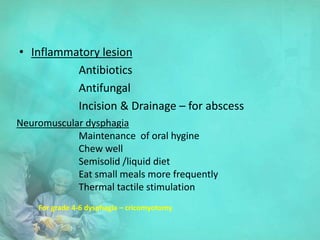
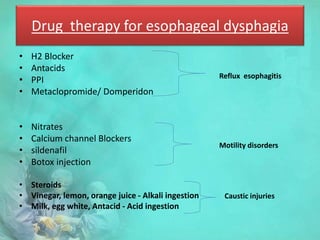
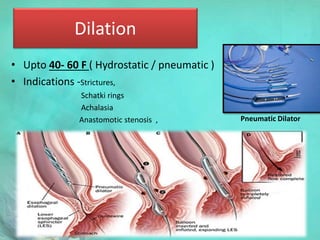
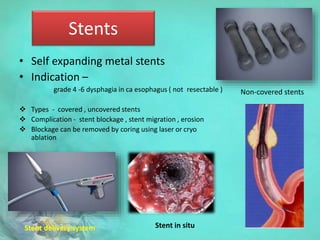
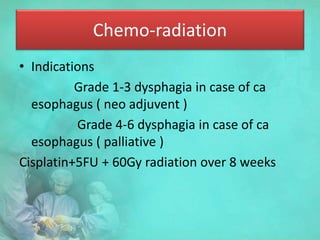
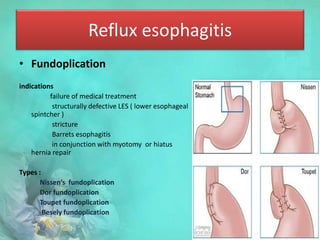
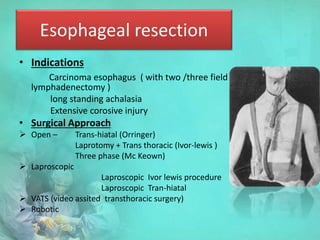
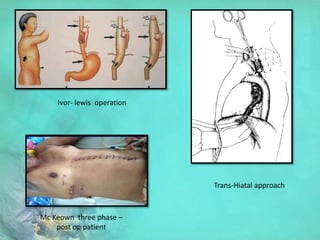
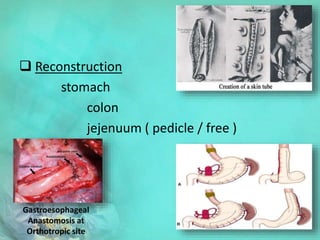
This document provides information on dysphagia (difficulty swallowing). It begins by defining dysphagia and describing the swallowing mechanism. The clinical presentation of dysphagia is then outlined. Dysphagia can be graded on a scale of 1 to 6 based on severity. The document discusses the main causes/etiologies of dysphagia as being neurological, mechanical/obstructive issues. Evaluation involves history, examination, imaging like barium swallow and endoscopy. Management depends on the underlying cause and may include lifestyle changes, medications, endoscopic procedures like dilation, stenting, or surgery.