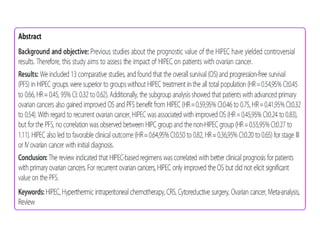
This document discusses hyperthermic intraperitoneal chemotherapy (HIPEC) plus cytoreductive surgery (CRS) for advanced ovarian cancer. A meta-analysis found that combining HIPEC with CRS improved both overall survival and progression-free survival compared to CRS alone. Subgroup analyses showed these benefits applied to both primary and recurrent ovarian cancer, including stage III and IV disease. The analysis provides emerging evidence that HIPEC combined with CRS and systemic chemotherapy improves outcomes over CRS and chemotherapy alone for treating ovarian cancer.
















![For CRS alone, the DESKTOP OVAR Trial showed that macroscopically
completely resected tumours showed significantly longer overall
survival compared to patients who had any visible residual tumour.
[median 45.2 vs. 19.7 months; hazard ratio (HR) 3.71; 95% confidence
interval (CI) 2.27-6.05; P < .0001]](https://image.slidesharecdn.com/hipecrct-200528145650/85/Hipec-_-meta-analysis-18-320.jpg)