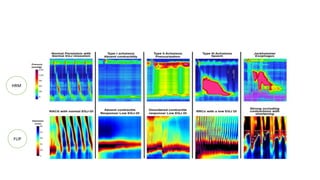
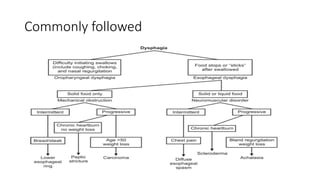
This document provides an overview of dysphagia (difficulty swallowing) including its causes, presentations, investigations, and management approaches. Dysphagia can result from problems in the oral, pharyngeal, or esophageal phases of swallowing. Common causes include strokes, neurological diseases, head and neck cancers. Investigations may include barium swallows, endoscopy, biopsy, and esophageal manometry. Newer techniques like high-resolution manometry and functional luminal imaging probe allow more detailed assessment of esophageal motility and function. Management is tailored to the underlying cause but may include dietary modifications, swallowing exercises, or medical/surgical interventions in severe cases.