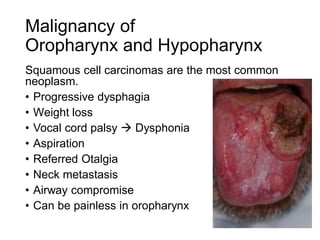
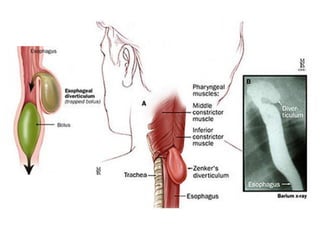
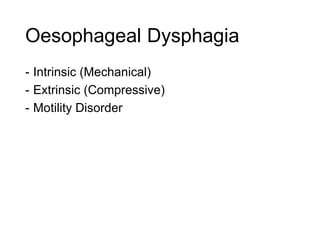
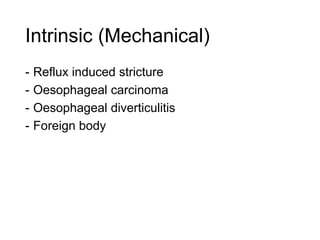
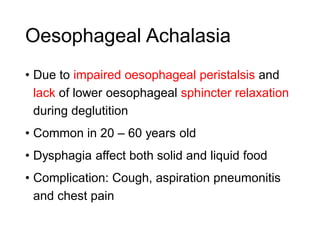
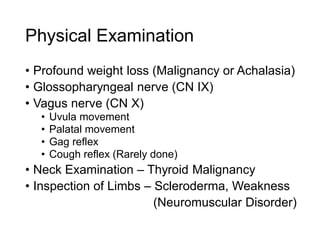
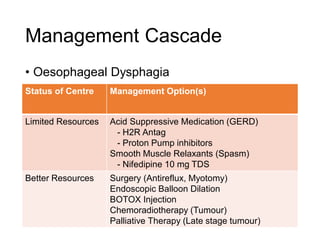
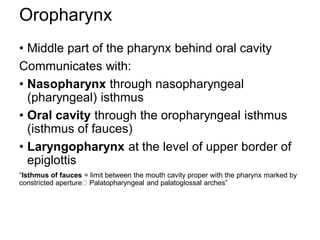
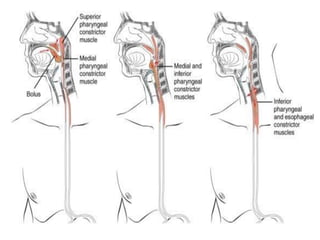
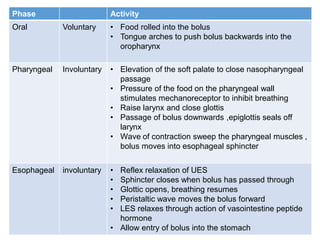
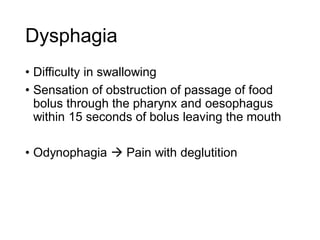
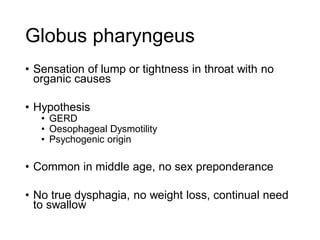
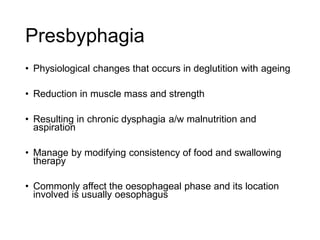
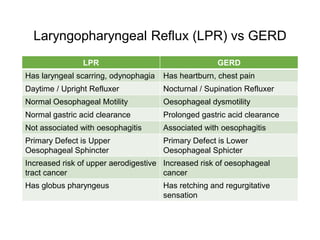
This document discusses dysphagia (difficulty swallowing) including its anatomy, physiology, causes, investigation, and management. It covers the anatomy of the oropharynx and hypopharynx. The physiology section describes the three phases of swallowing - oral, pharyngeal, and esophageal. Common causes of dysphagia include presbyphagia, laryngopharyngeal reflux, xerostomia, tonsillitis, epiglottitis, oropharyngeal/hypopharyngeal malignancies, and pharyngeal pouches. Investigations include endoscopy, barium swallow, and manometry. Management is tailored based on the cause and resource availability,


















![Oropharyngeal Dysphagia
- Difficulty initiating deglutition
- Associated with coughing, choking, regurgitation,
aspiration, sensation of food in the pharynx
- Pathological site
- Oropharynx
- Oral dysfunction signs
- Drooling of saliva
- Hypersalivation (Sialorrhea)
- [Reason: compensatory mechanism for dysphagia]
- Piecemeal swallow
- Pharyngeal dysfunction signs
- Coughing
- Choking
- Regurgitation](https://image.slidesharecdn.com/group4-dysphagia2016version3-160302032559/85/Group-4-dysphagia-2016-version-3-1-validated-28-320.jpg)