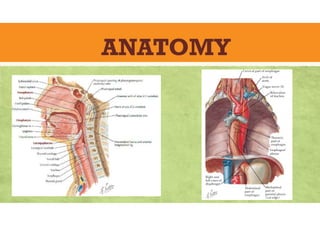
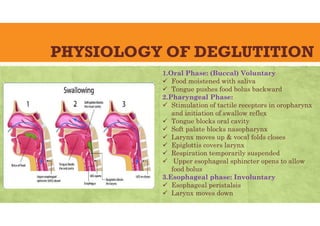
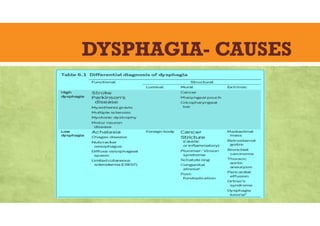
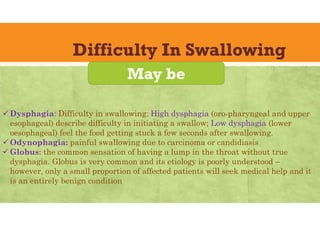
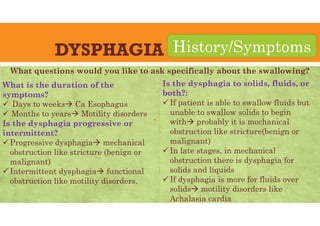
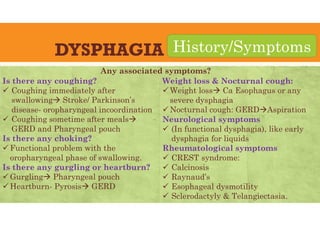
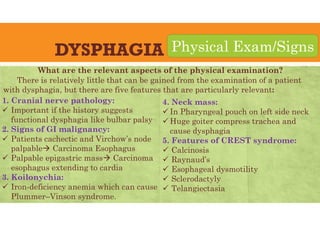
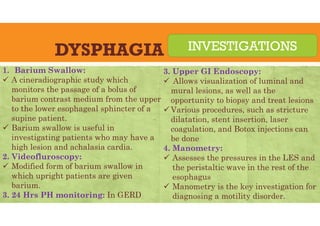
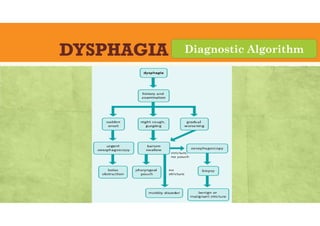
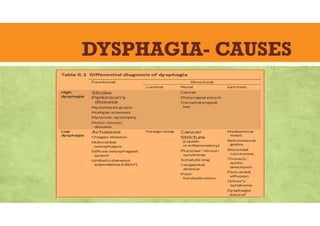
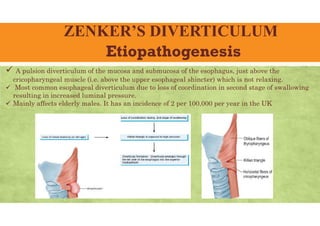
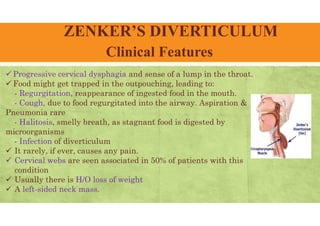
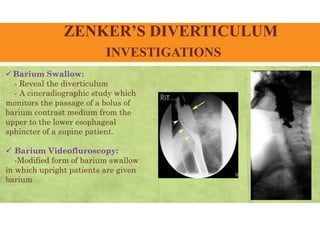
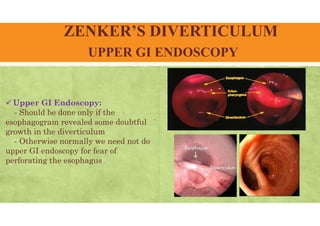
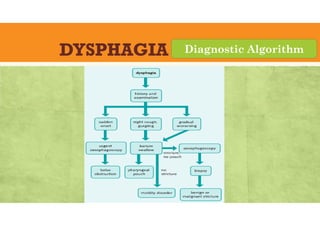
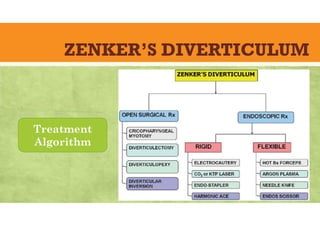
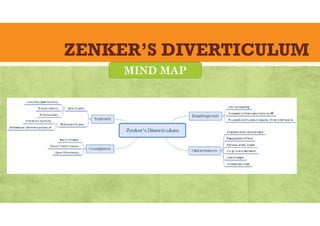
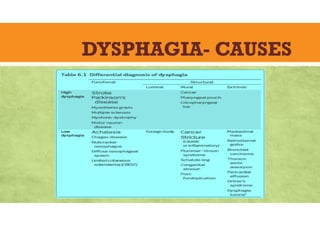
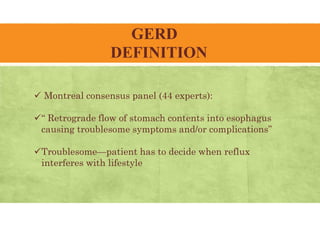
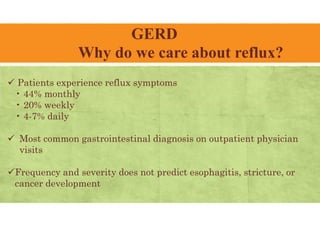
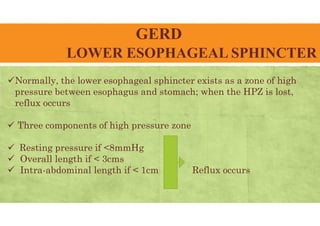
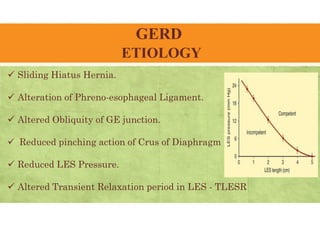
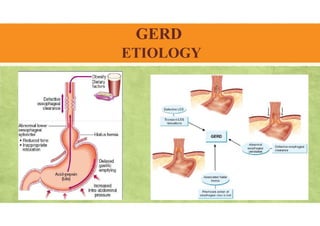
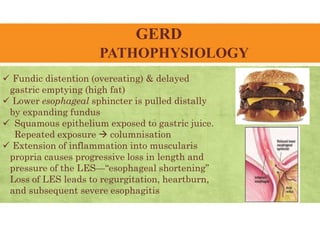
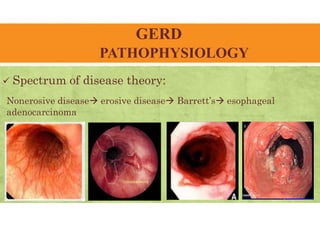
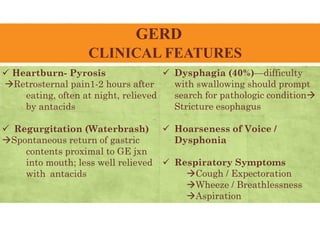
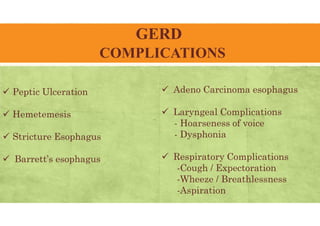
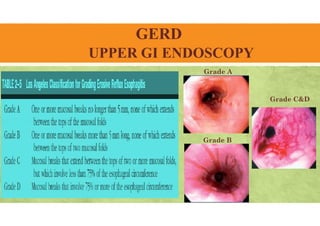
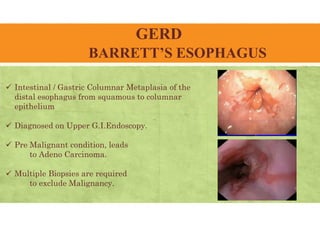
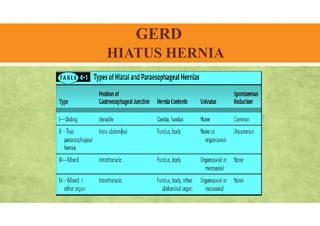
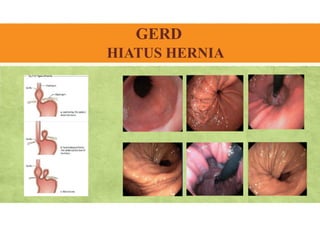
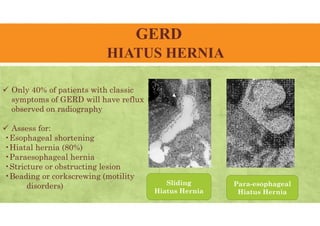
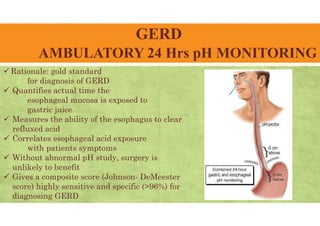
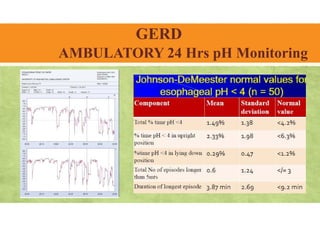
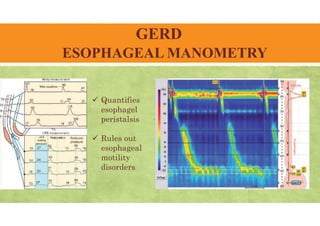
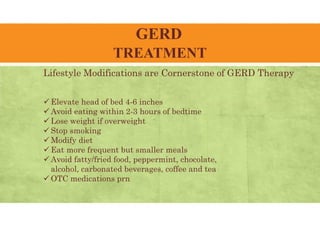
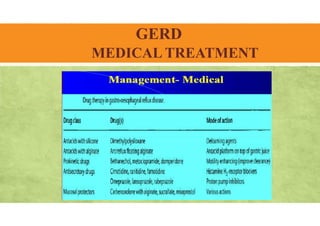
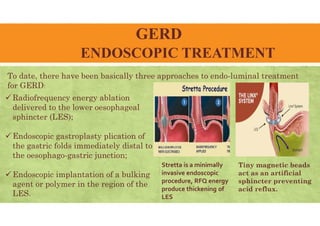
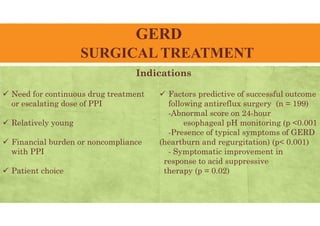
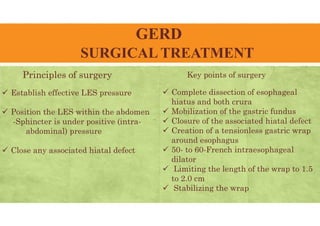
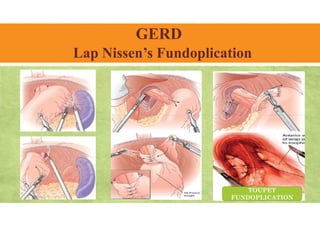
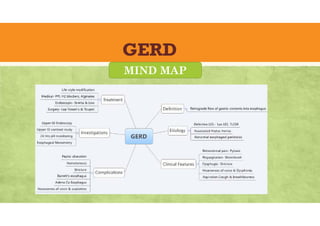
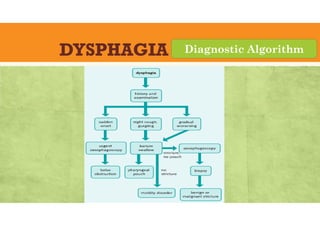
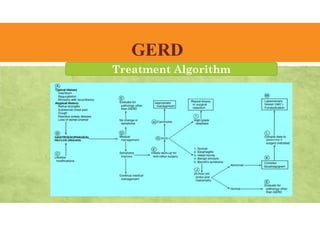
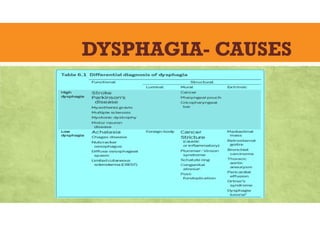
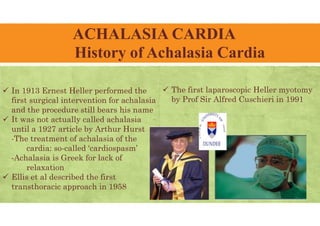
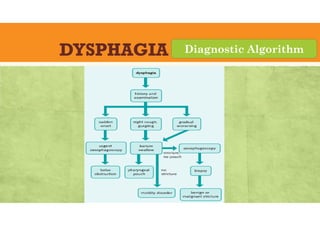
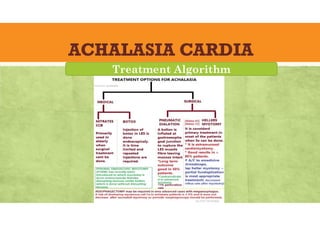
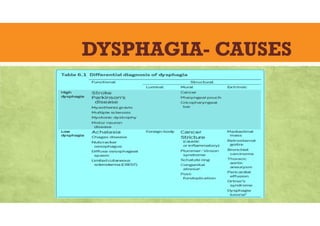
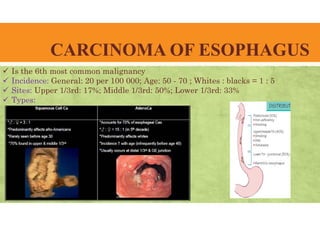
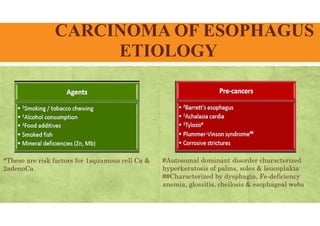
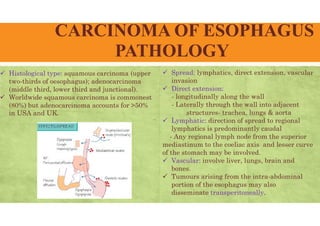
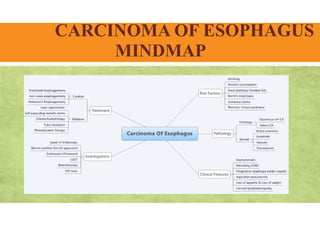
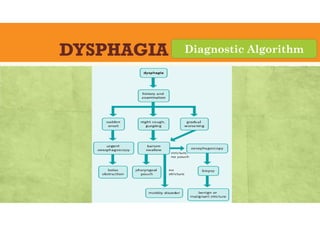
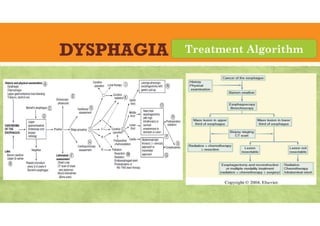
The document provides an overview of dysphagia, including its definition, anatomy and physiology of swallowing, causes, history, symptoms, physical examinations, investigations, and diagnostic algorithms. Additionally, it discusses specific conditions such as Zenker's diverticulum and gastroesophageal reflux disease (GERD), outlining their clinical features, diagnostic procedures, and treatment approaches. Overall, it emphasizes the importance of understanding dysphagia for effective diagnosis and management in surgical practice.