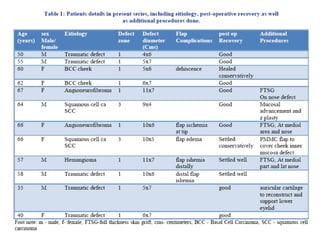
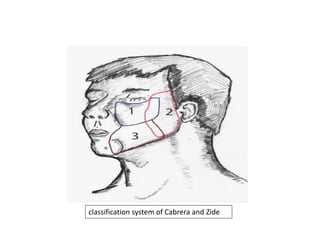
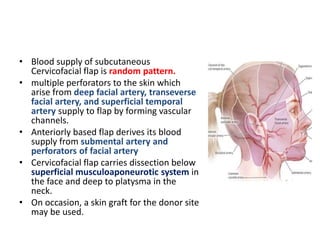
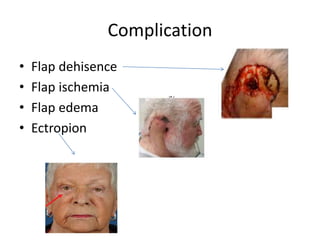
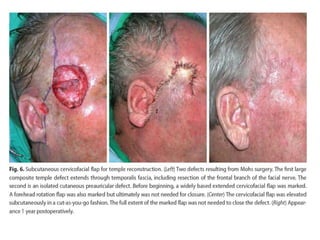
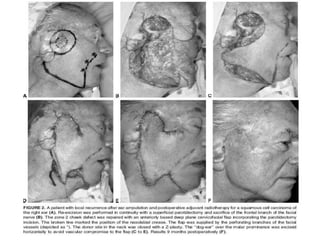
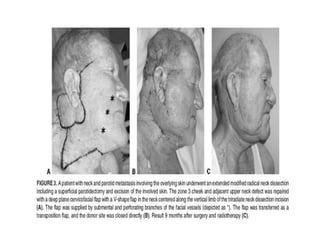
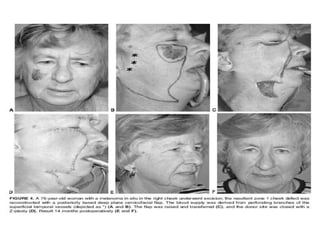
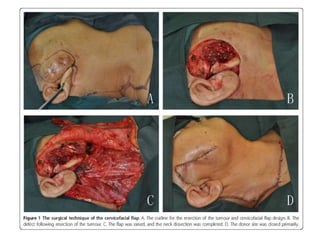
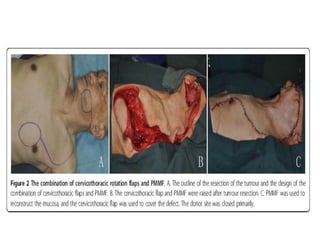
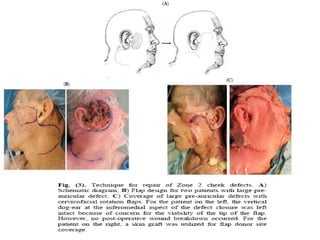
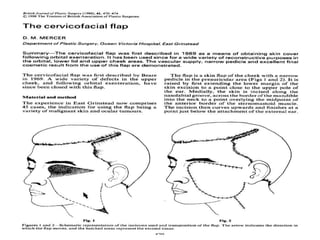
This document discusses a prospective study involving 12 patients aimed at evaluating the effectiveness of cervicofacial flaps for reconstructing cheek defects. It highlights the advantages of the technique, including reduced surgical risks for high-risk patients and short operative times, and also identifies potential complications such as flap dehiscence and ischemia. The study categorizes cheek defects based on their size and location, suggesting appropriate reconstruction methods for each category.