This document discusses diabetic retinopathy, including:
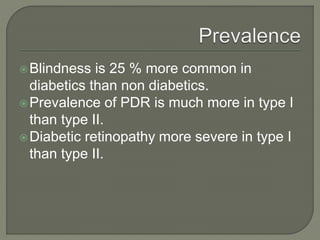
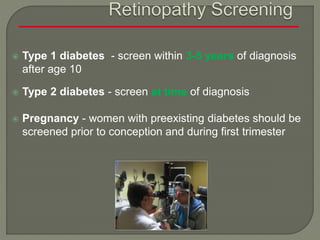
- The two main types of diabetes and how they relate to retinopathy risk and onset age.
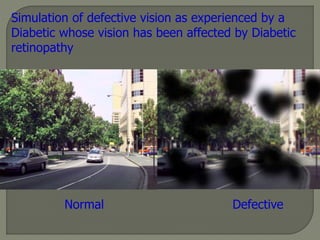
- Diabetic retinopathy as a leading cause of blindness and its impact.
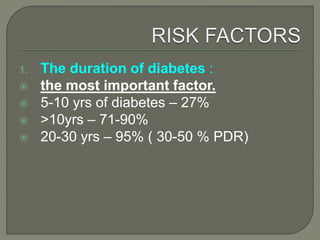
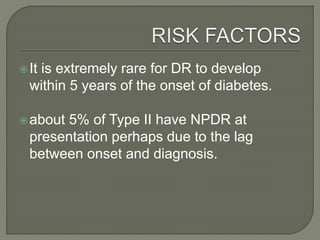
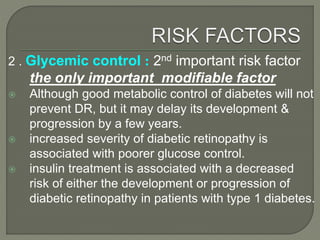
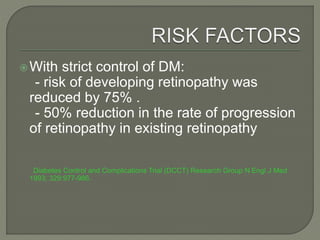
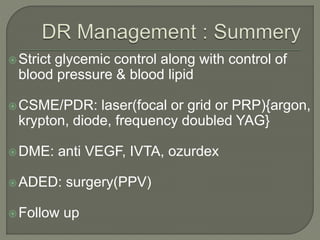
- Key risk factors like diabetes duration, glycemic control, and other systemic factors.
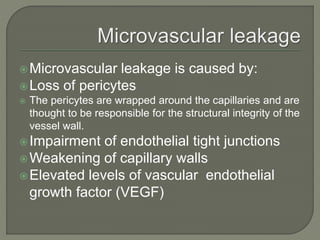
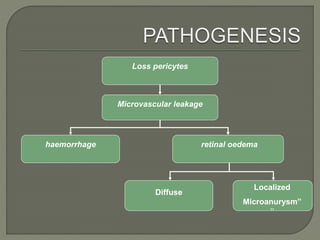
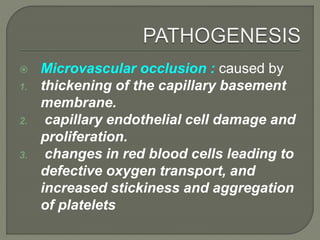
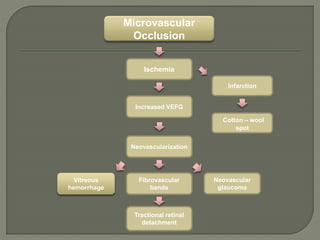
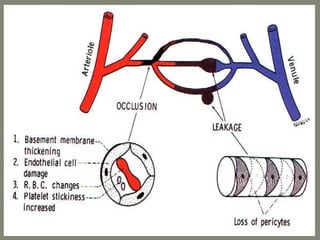
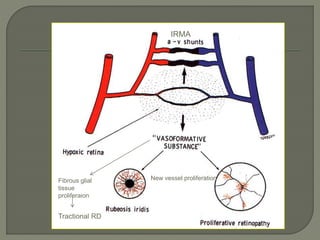
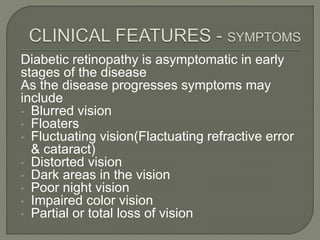
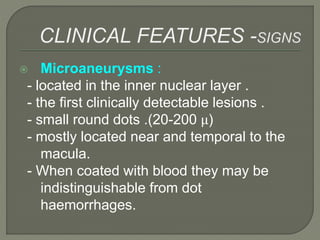
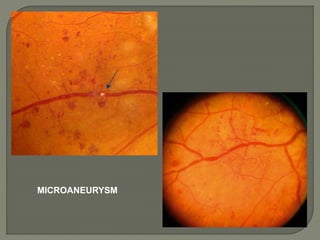
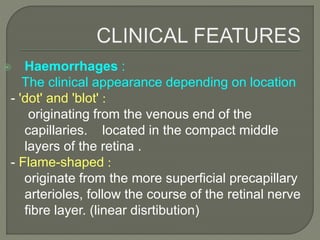
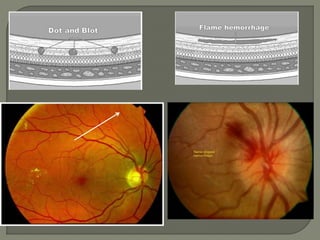
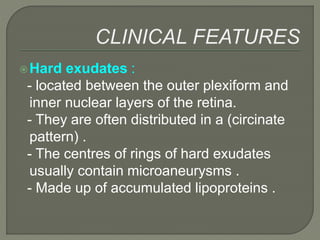
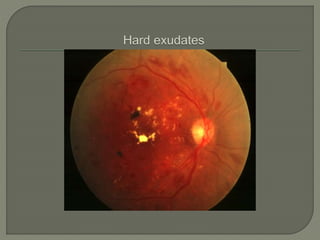
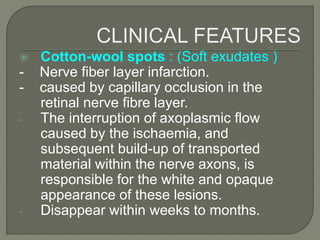
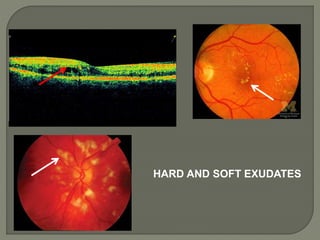
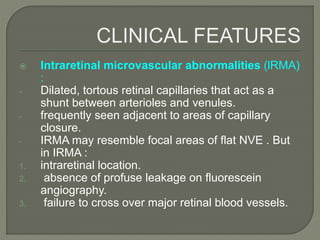
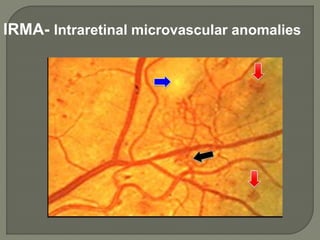
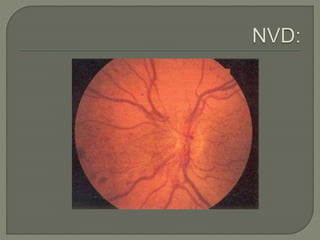
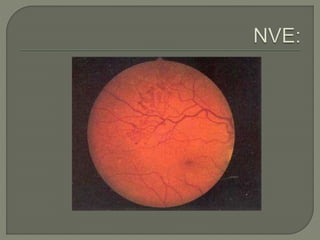
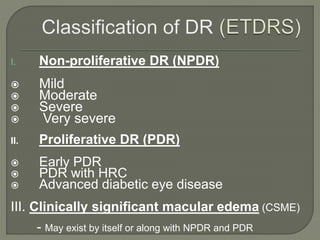
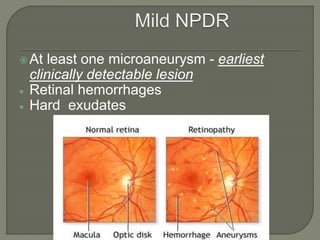
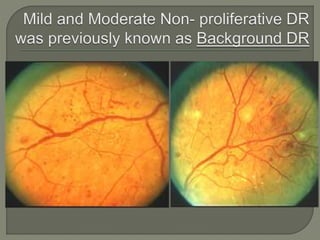
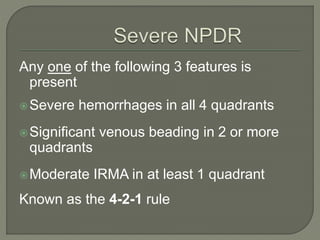
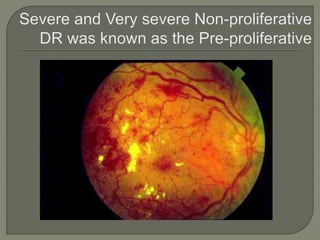
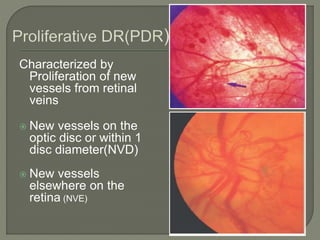
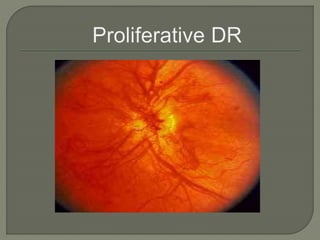
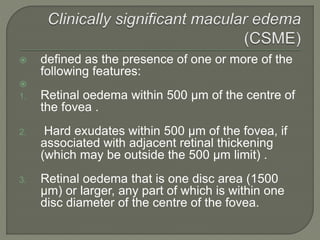
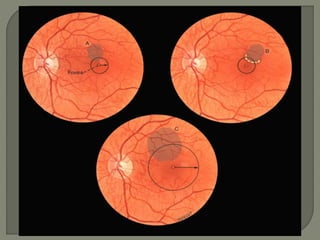
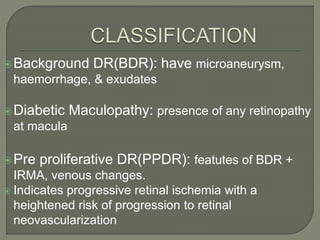
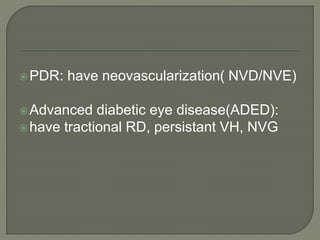
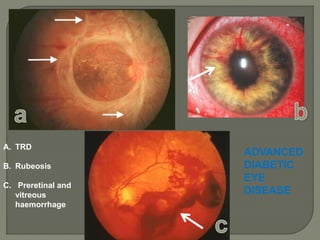
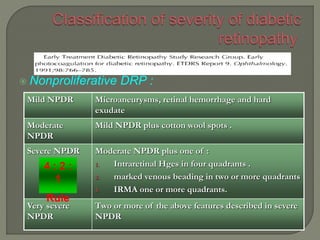
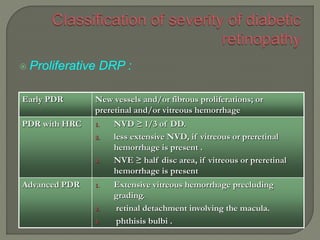
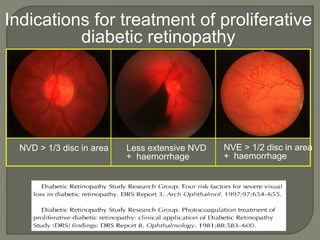
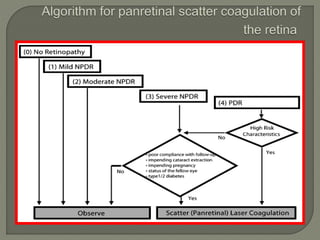
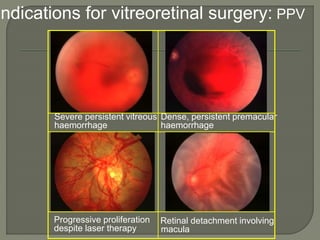
- The characteristic lesions and stages of non-proliferative and proliferative retinopathy.
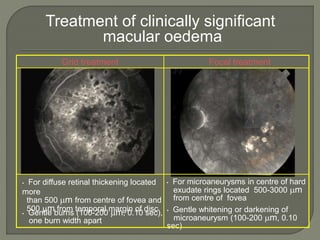
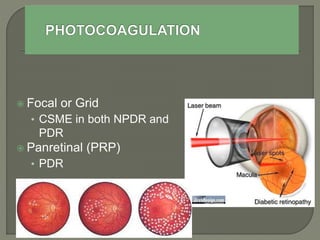
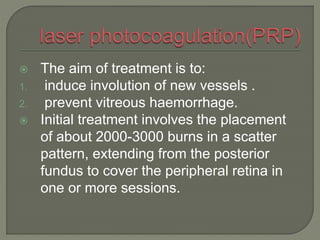
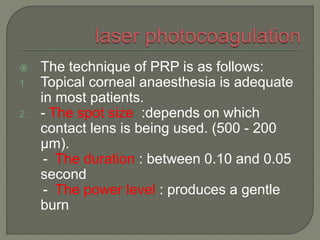
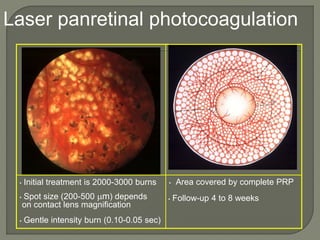
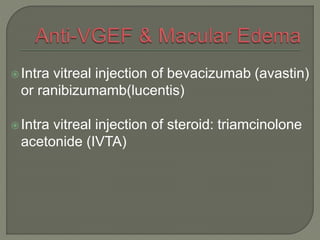
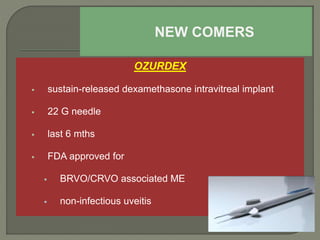
- Treatment approaches including laser photocoagulation, anti-VEGF injections, steroids, and surgery.
- Screening guidelines based on diabetes type and risk level.