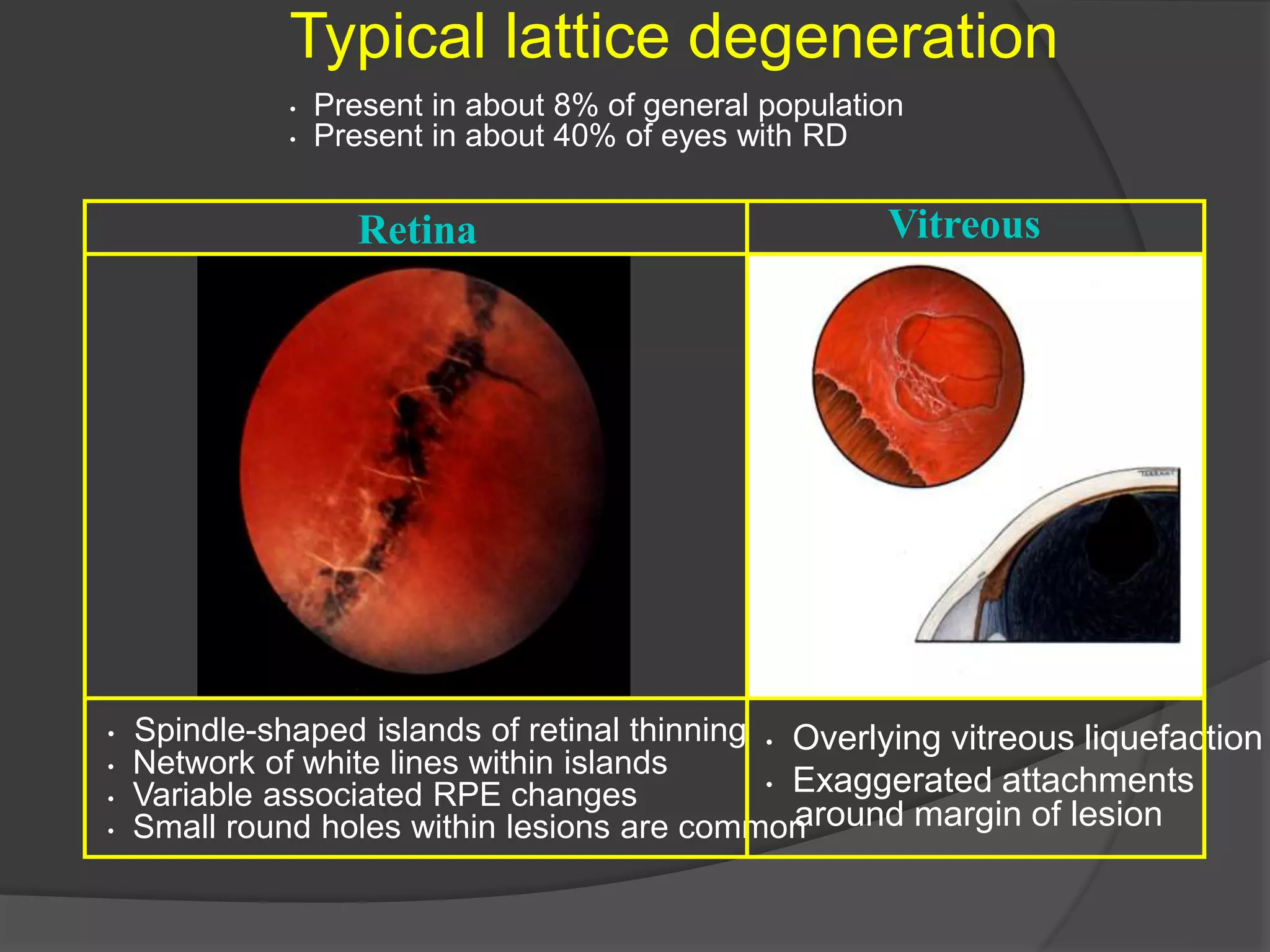
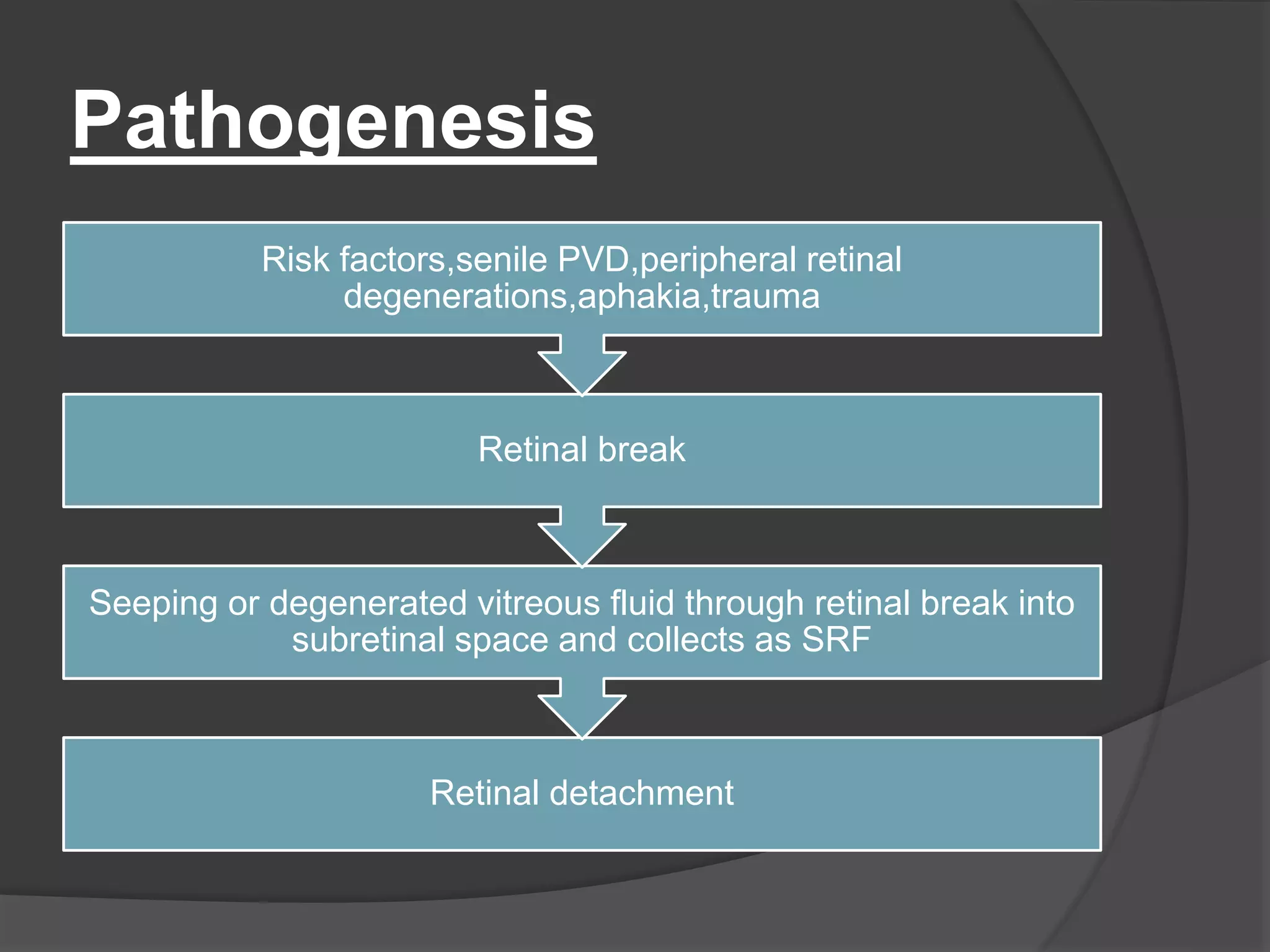
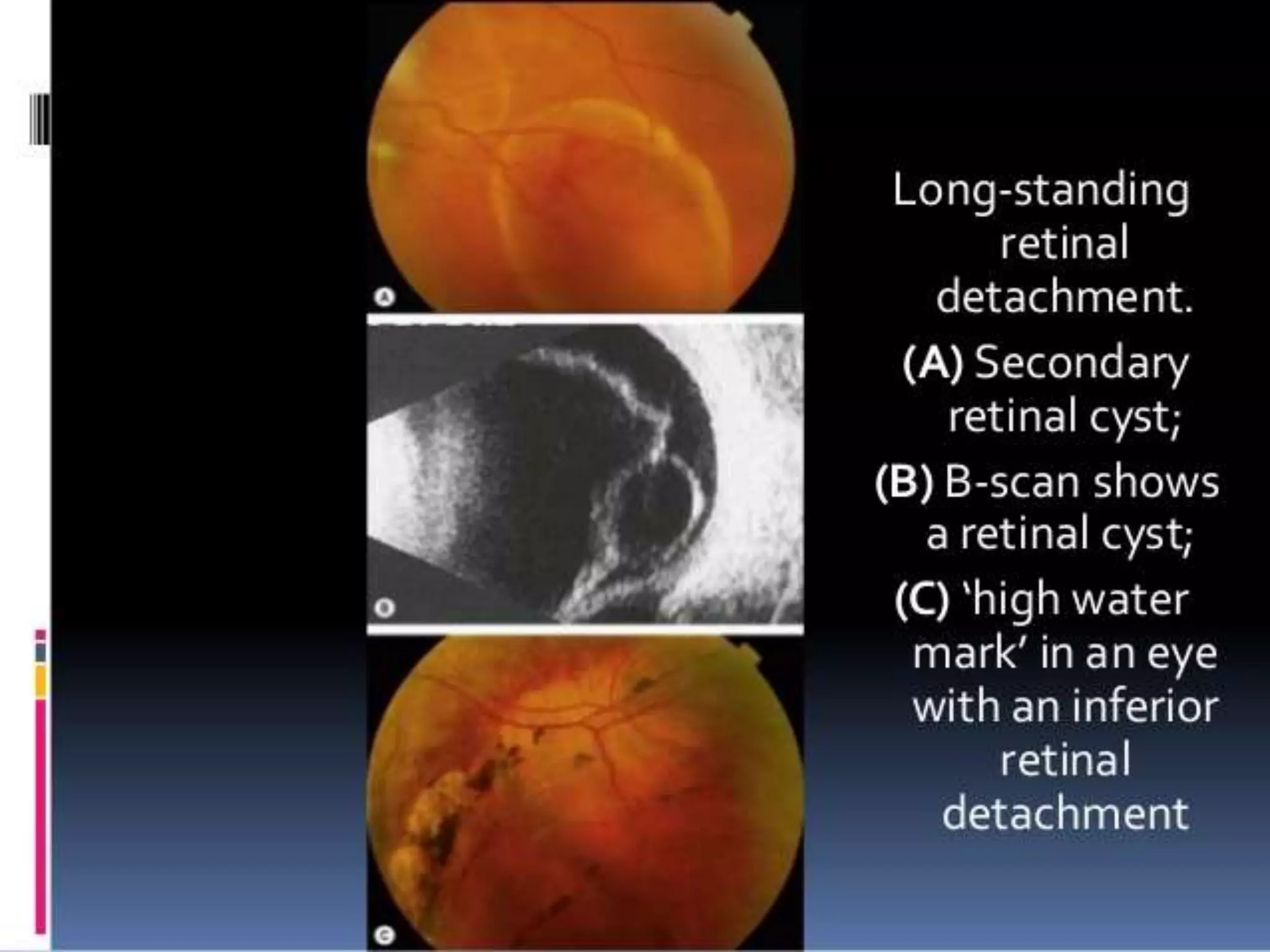
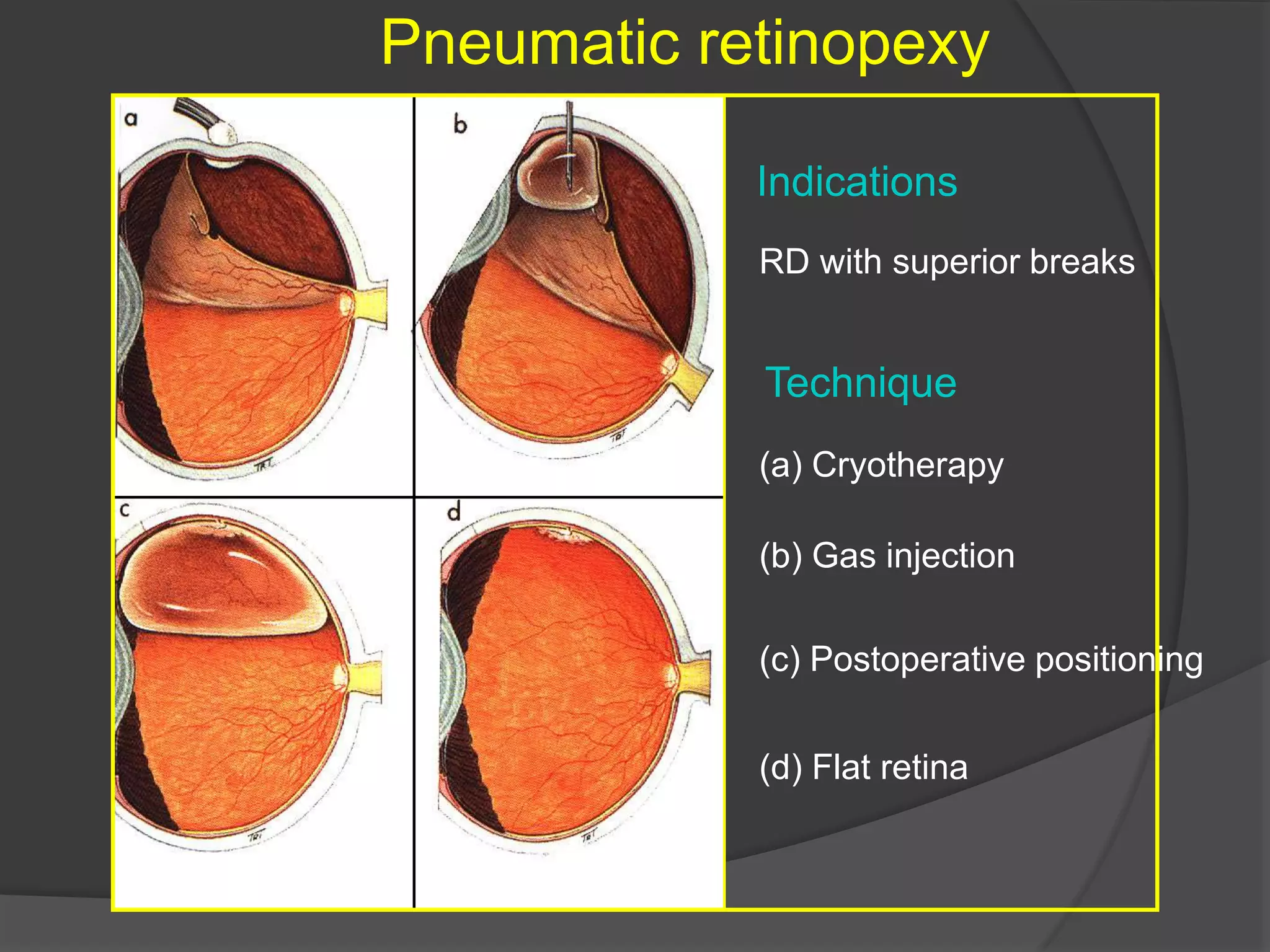
This document discusses retinal detachment and its treatment. There are four main types of retinal detachment: rhegmatogenous, tractional, exudative, and combined rhegmatogenous and tractional. Rhegmatogenous retinal detachment is caused by a break or tear in the retina that allows vitreous fluid to enter the subretinal space. Treatments include sealing retinal breaks through cryotherapy, laser photocoagulation, or scleral buckling surgery to maintain chorioretinal apposition. More advanced cases may require pars plana vitrectomy for membrane peeling and internal tamponade with long-acting gas or silicone oil.