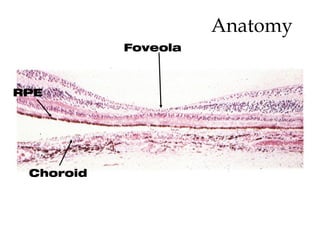
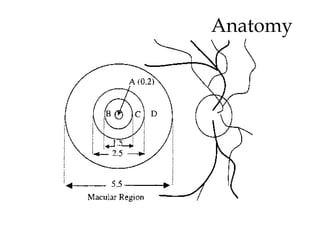
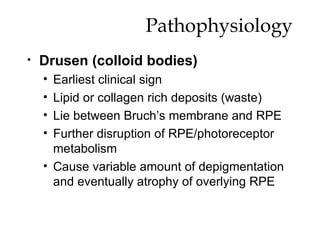
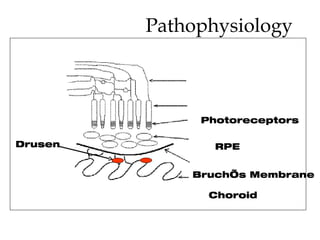
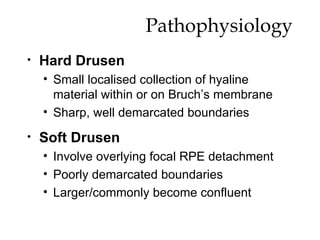
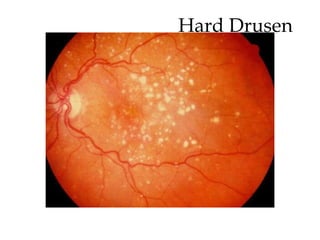
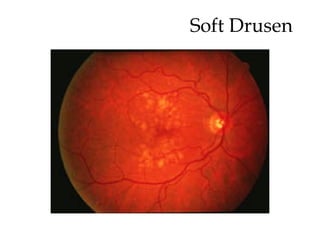
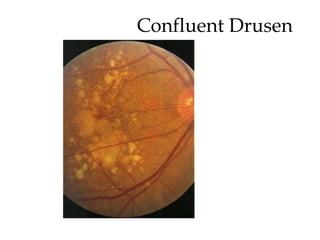
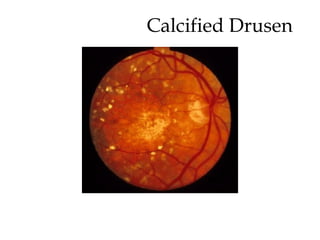
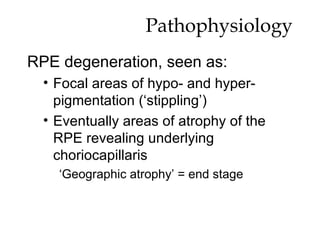
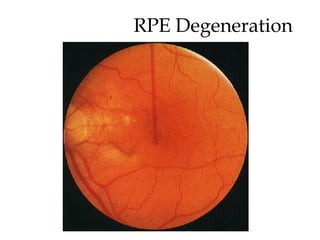
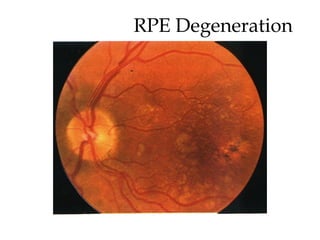
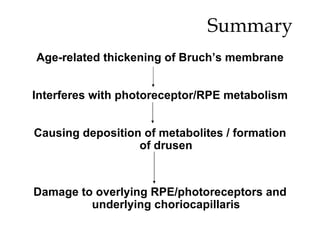
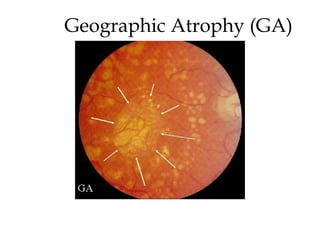
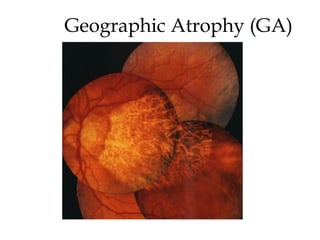
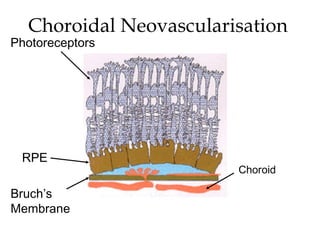
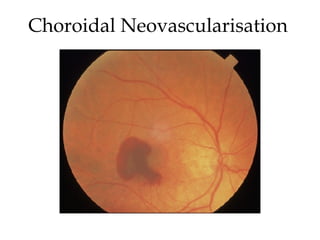
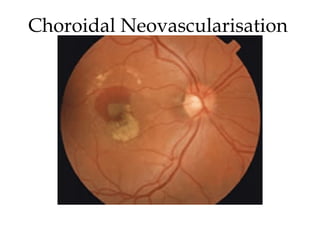
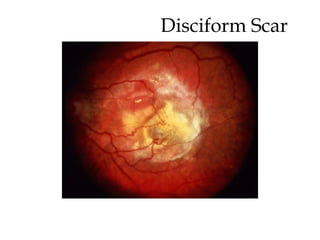
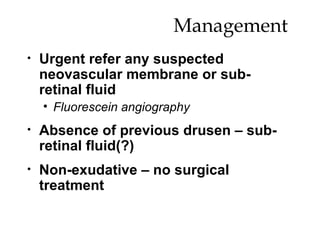
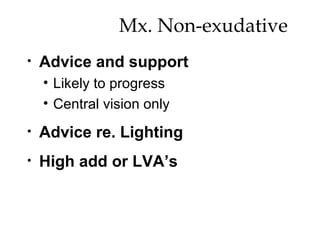
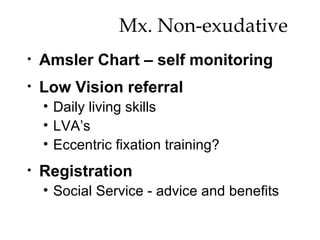
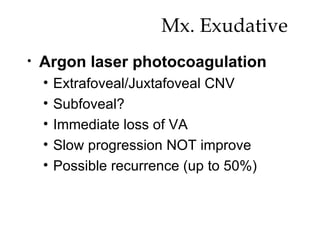
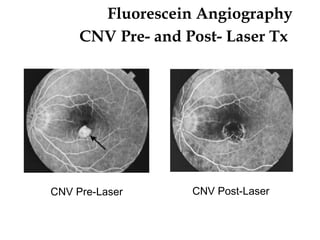
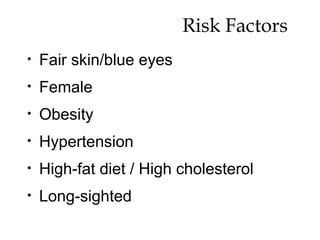
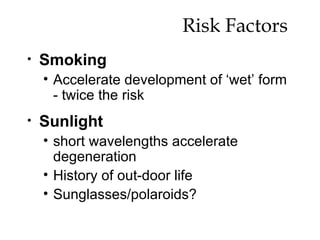
Age-related macular degeneration (AMD) is a leading cause of blindness that results from thickening of Bruch's membrane with age, interfering with metabolism in the retinal pigment epithelium (RPE) and photoreceptors. This causes deposits called drusen that damage the overlying RPE and underlying tissue. There are two forms: dry AMD involves gradual RPE and photoreceptor atrophy, while wet AMD features choroidal neovascularization that leaks fluid and blood, causing rapid vision loss if untreated. Risk factors include age, genetics, smoking, and diet.