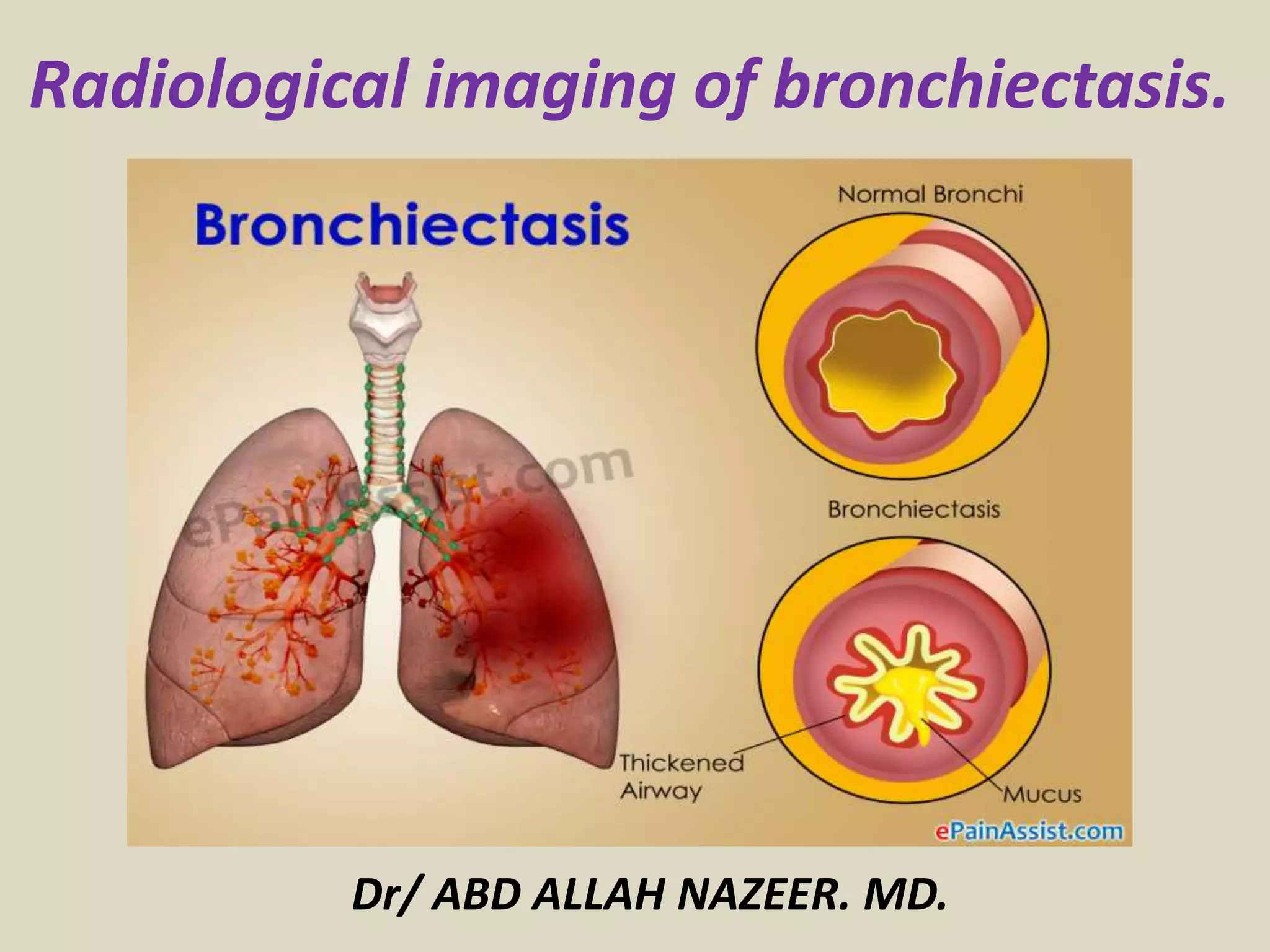
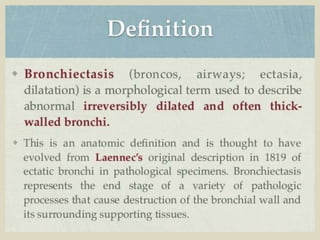
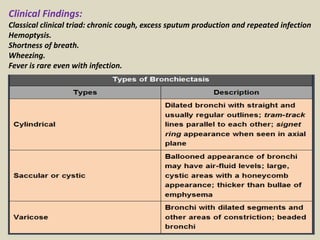
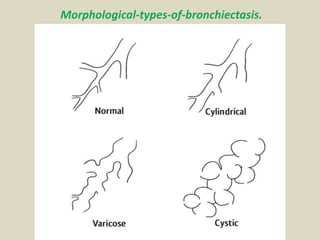
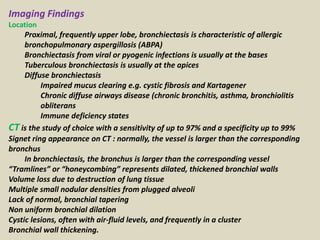
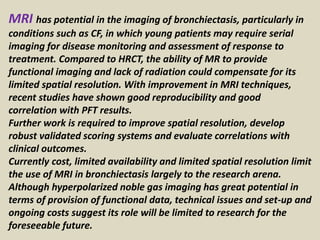
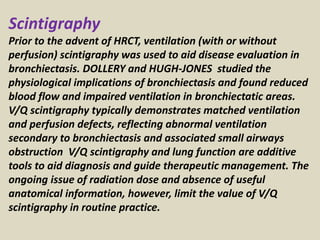
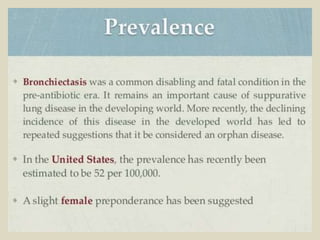
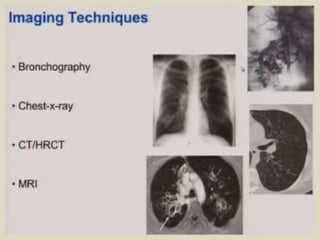
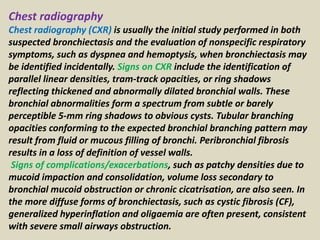
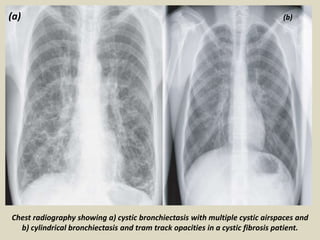
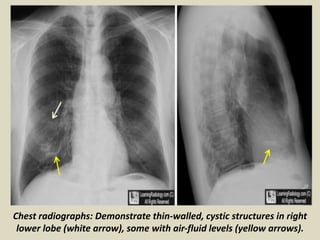
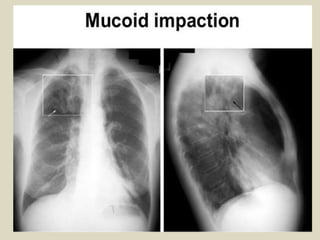
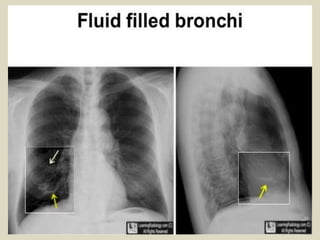
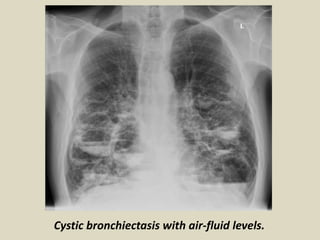
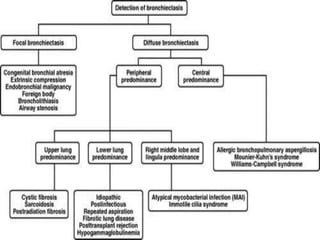
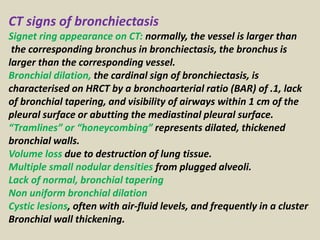
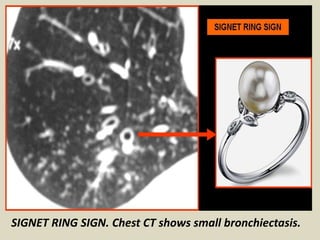
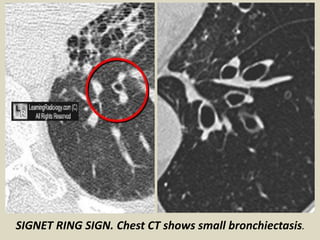
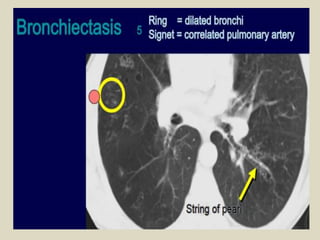
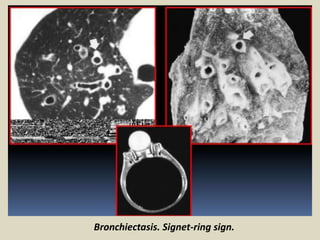
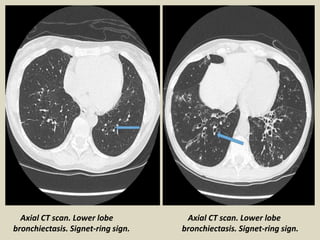
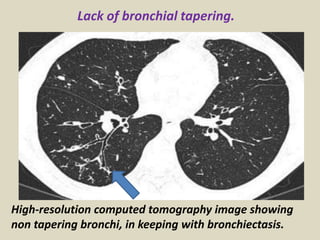
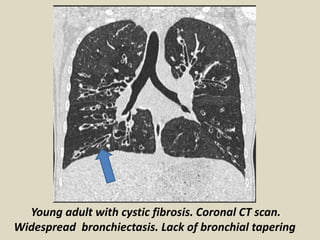
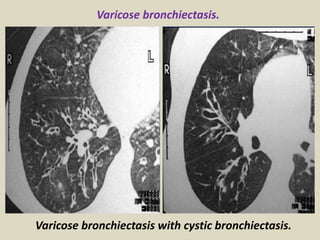
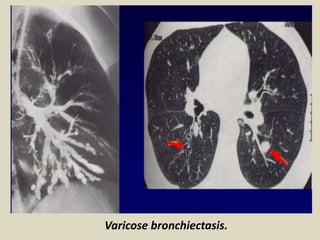
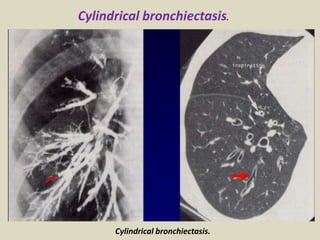
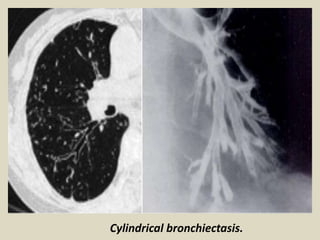
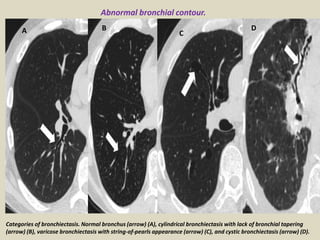
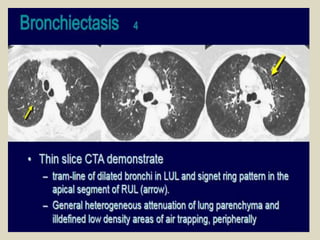
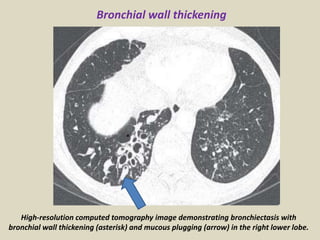
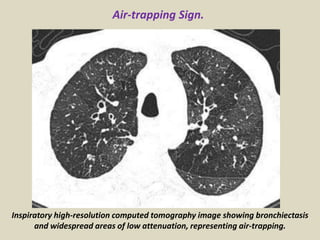
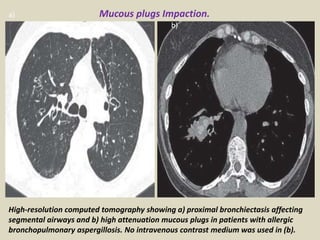
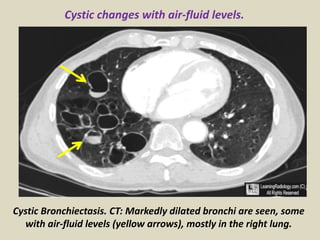
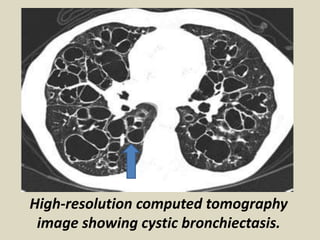
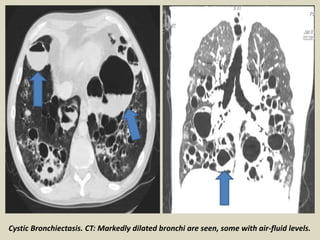
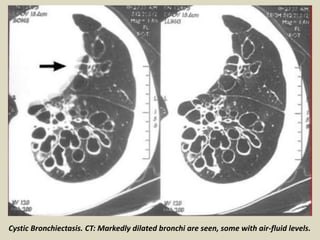
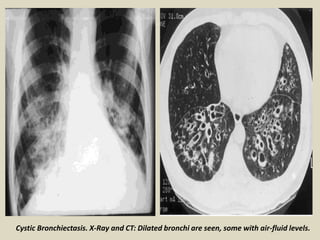
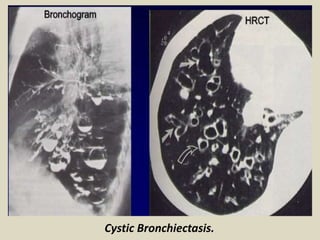
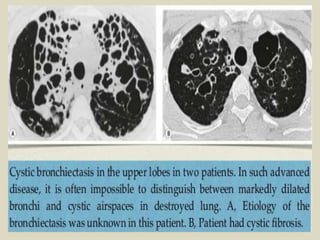
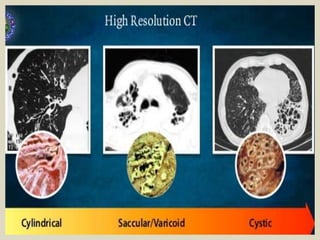
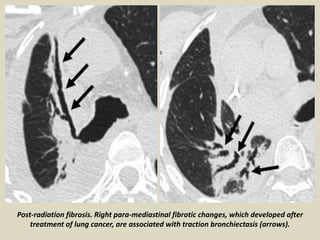
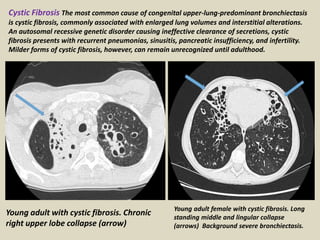
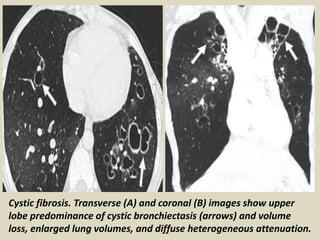
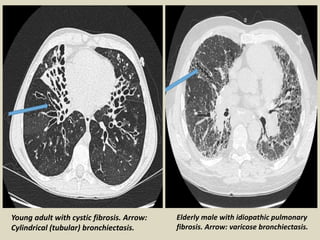
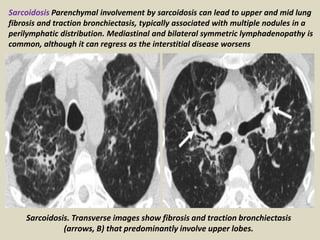
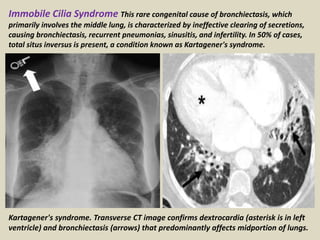
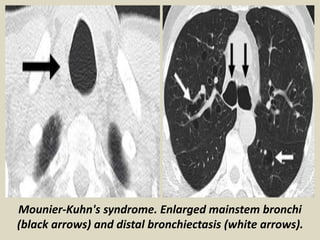
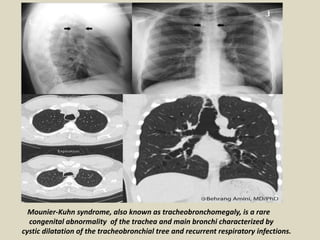
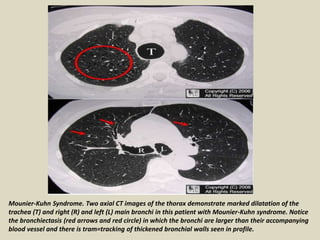
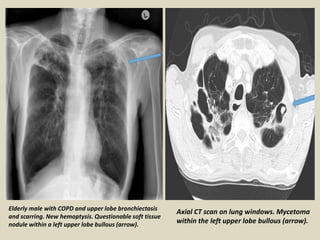
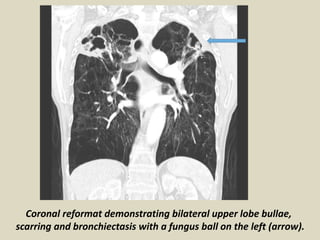
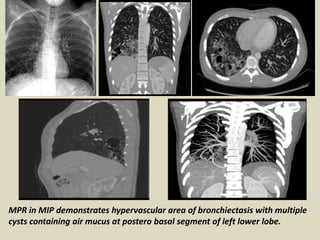
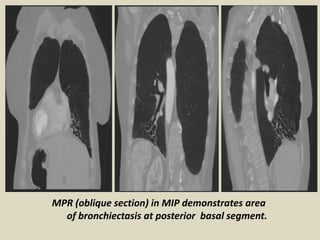
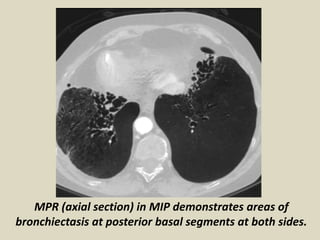
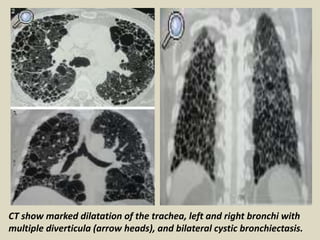
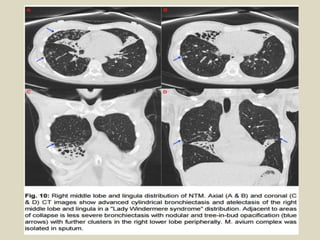
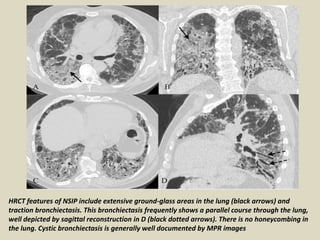
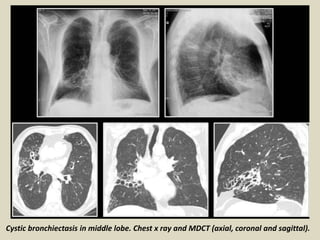
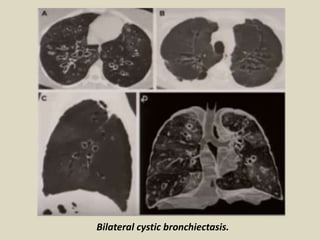
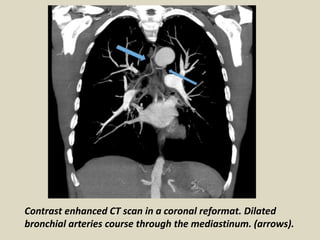
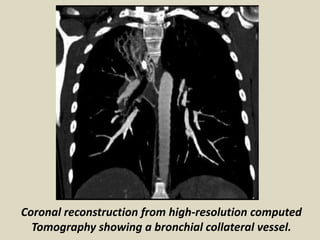
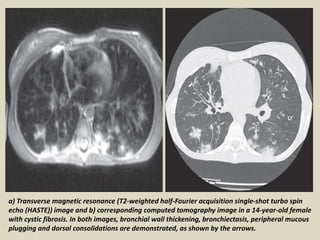
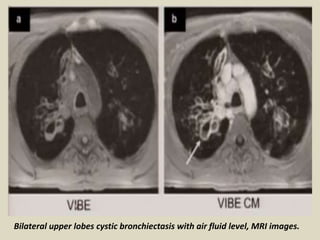
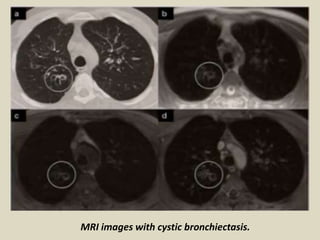
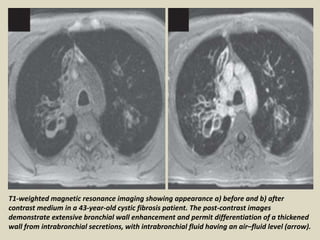
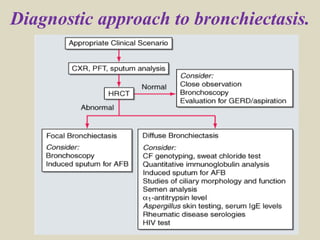
Radiological imaging plays an important role in diagnosing and characterizing bronchiectasis. CT scanning is the most sensitive imaging method, allowing visualization of bronchial dilation, lack of tapering, wall thickening, mucus plugging, and cyst formation. Different patterns of bronchiectasis exist, including cylindrical, varicose, and cystic forms. Underlying causes like cystic fibrosis or post-infectious processes are often associated with specific locations of bronchiectasis within the lungs. Other imaging modalities like MRI, scintigraphy, and chest x-rays can provide supplemental information but have limitations compared to CT.