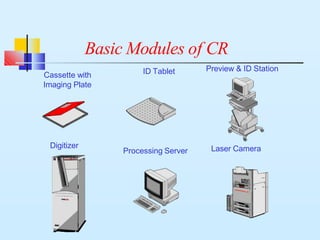
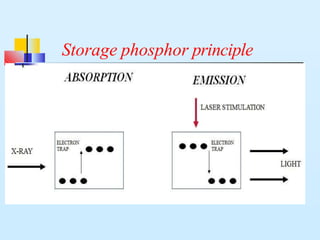
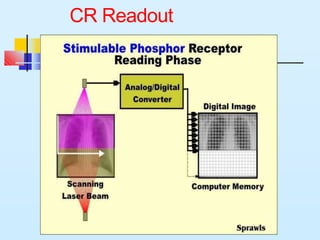
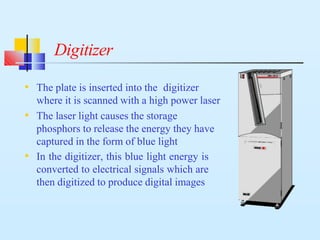
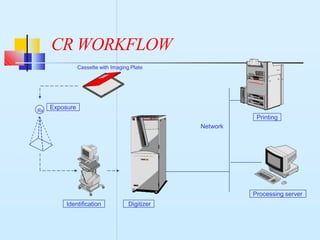
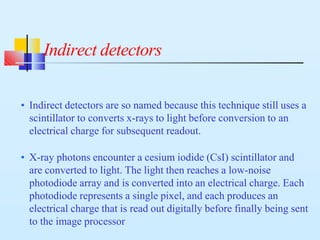
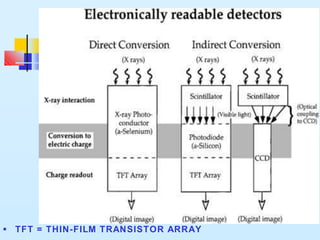
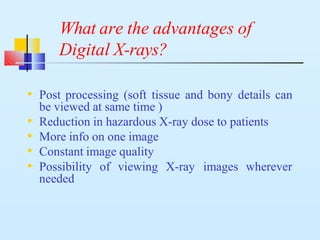
Computed radiography and digital radiography are two methods for obtaining digital x-rays. Computed radiography uses an imaging plate inside a cassette that captures x-rays, which are then digitized in a CR reader. Digital radiography uses a flat panel detector with either direct or indirect conversion of x-rays to electrical signals. Both methods provide advantages over conventional film such as faster workflow, ability to adjust images after exposure, and reduced radiation dose for patients.