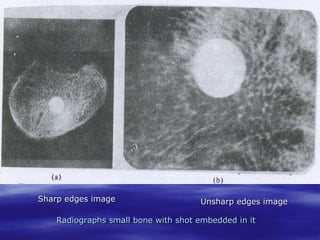
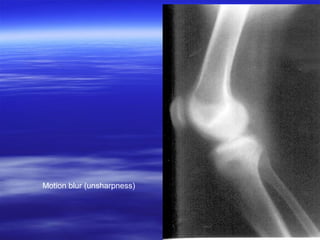
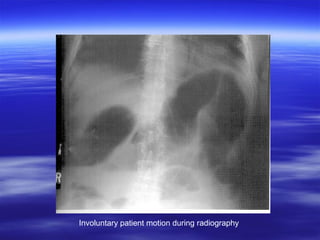
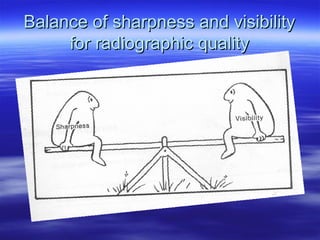
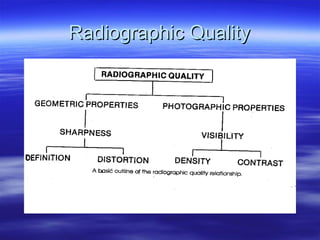
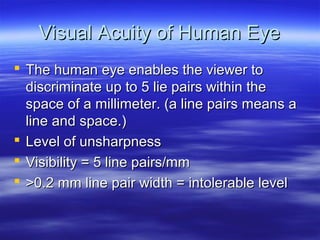
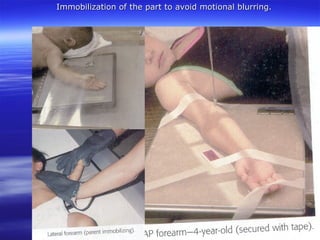
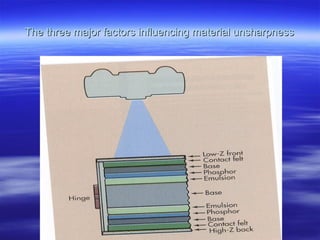
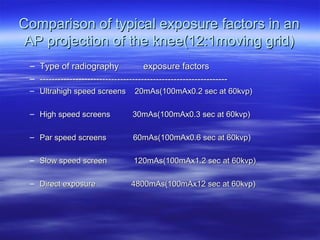
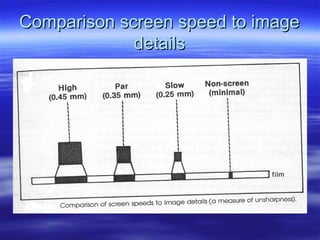
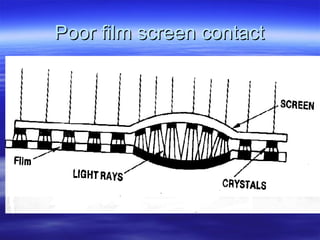
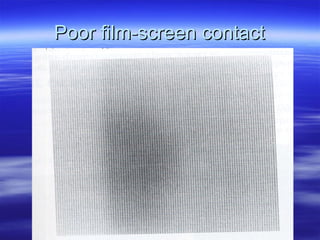
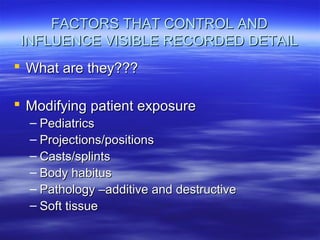
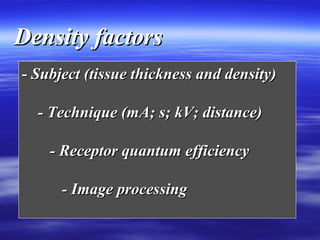
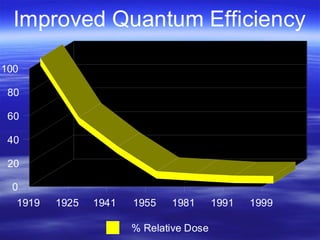
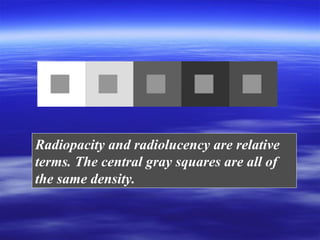
The document discusses key factors that contribute to radiographic image quality, including sharpness and visibility. Sharpness refers to the ability to clearly define edges and is influenced by factors like motion blur and material properties. Visibility refers to the distinguishability of distant objects and depends on density and contrast, which are also important quality metrics. Obtaining diagnostic images with both sharpness and visibility while minimizing radiation exposure requires consideration of numerous technical parameters like screen speed, mAs, kVp, and immobilization techniques. An optimal radiographic technique balances all relevant image quality attributes.