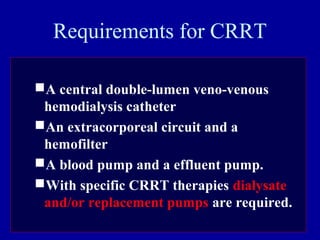
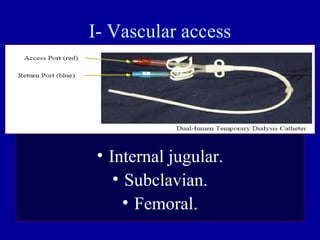
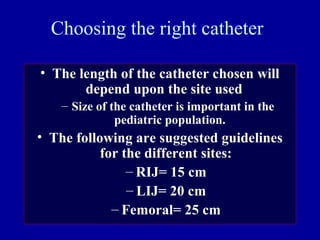
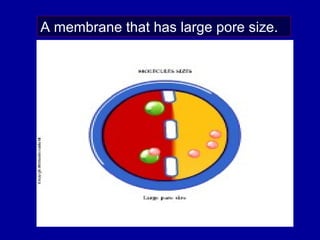
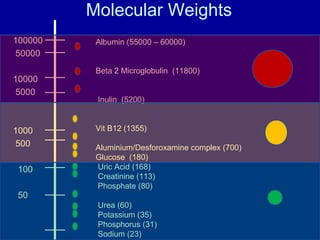
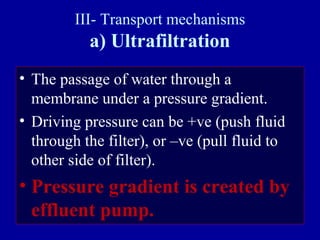
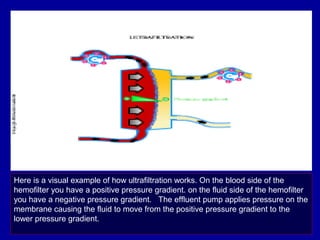
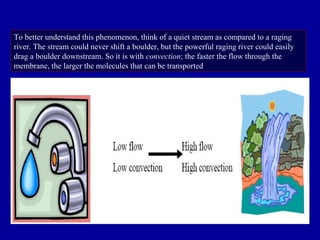
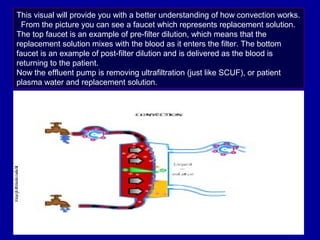
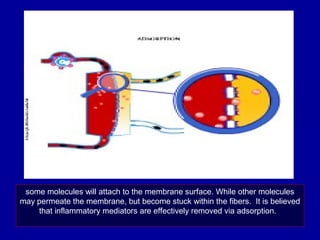
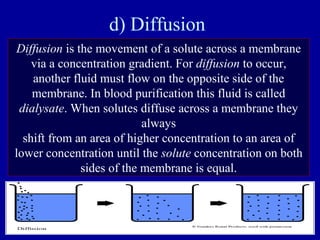
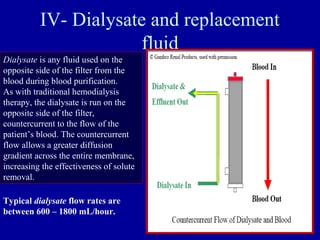
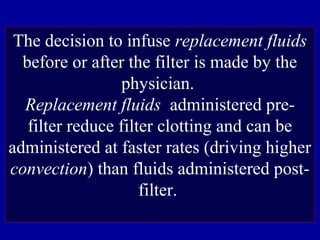
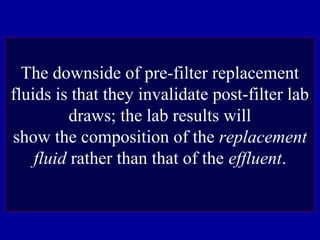
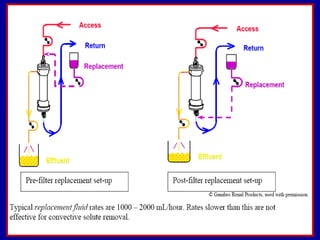
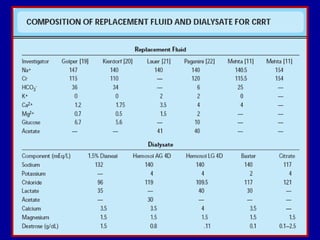
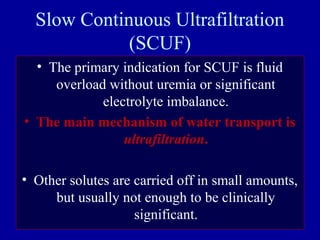
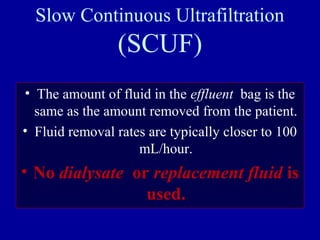
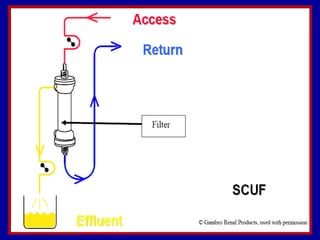
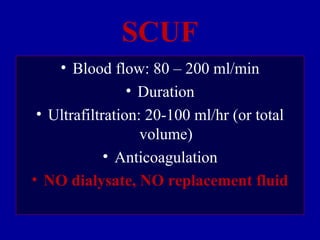
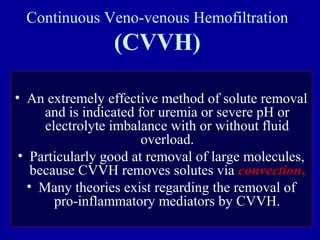
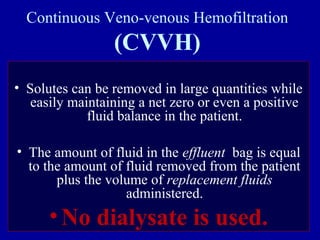
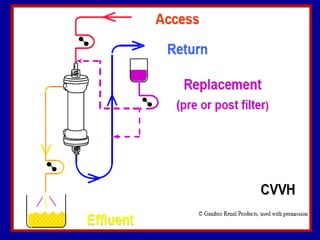
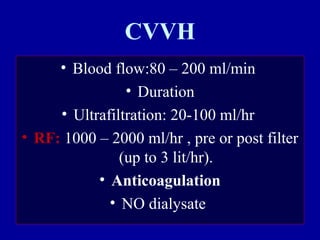
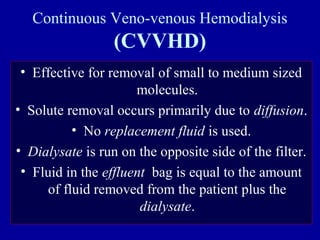
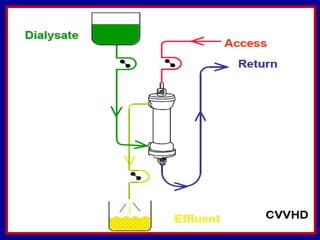
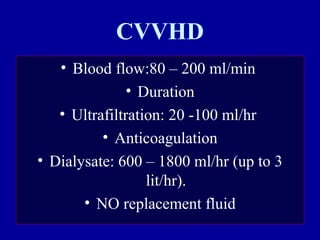
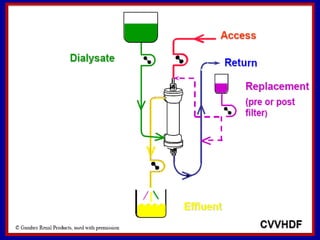
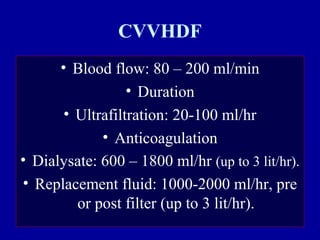
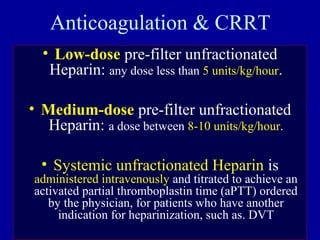
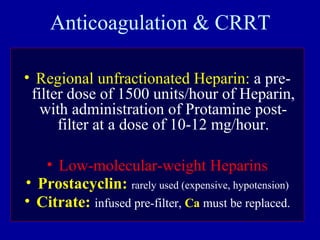
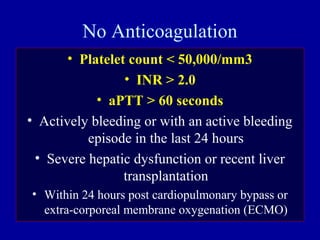
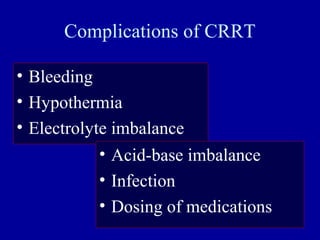
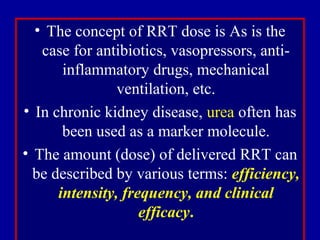
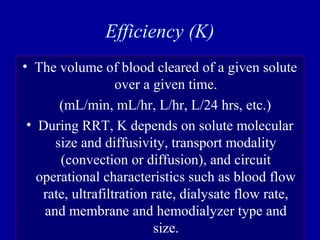
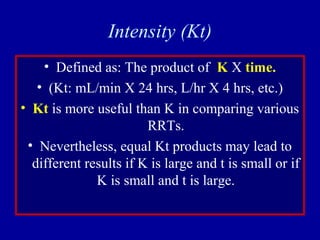
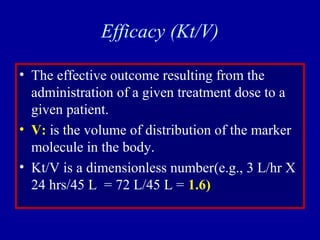
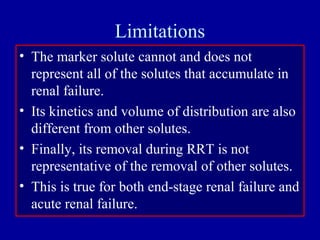
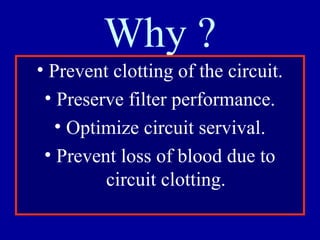
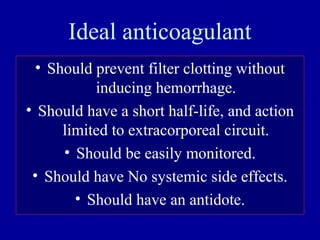
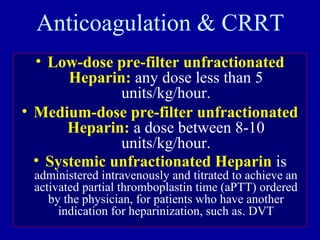
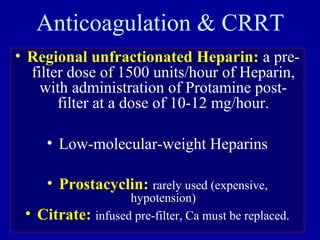
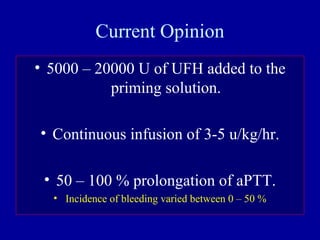
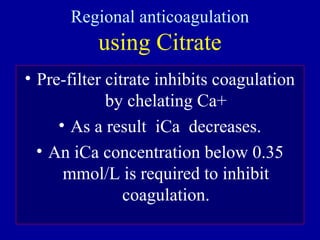
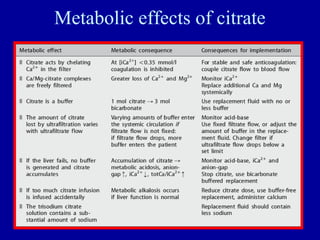
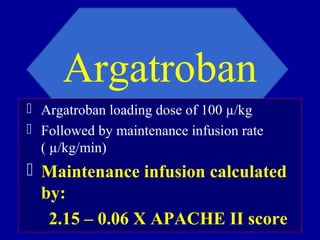
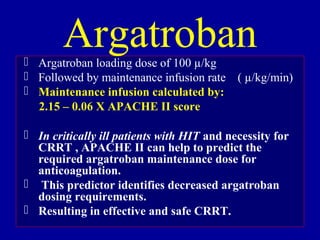
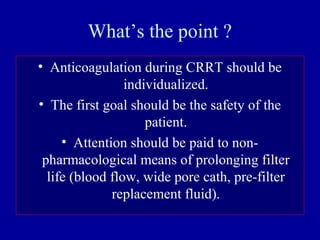
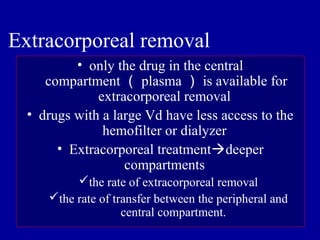
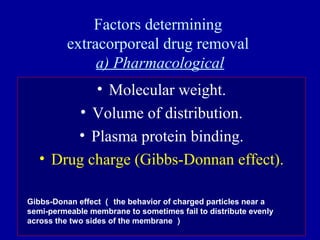
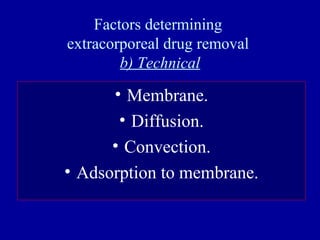
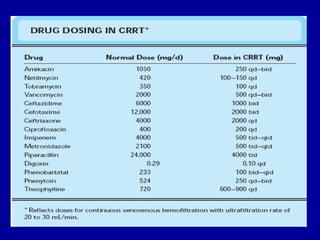
This document discusses continuous renal replacement therapy (CRRT). It defines CRRT as an extracorporeal blood purification therapy intended to substitute impaired renal function over an extended period of 24 hours. It describes the requirements, indications, principles, and modalities of CRRT including vascular access, semi-permeable membranes, transport mechanisms, dialysate, replacement fluids, and different types of CRRT like CVVH, CVVHD, and CVVHDF. It also discusses dosing of CRRT, anticoagulation methods, and some complications.