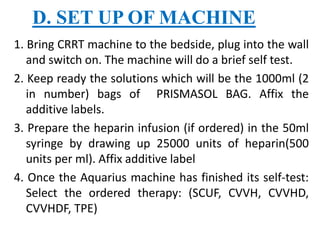
This document provides information about continuous renal replacement therapies (CRRT). It begins by explaining that CRRT is a type of hemodialysis used for critically ill patients with acute or chronic kidney failure. CRRT circulates blood through a filter and slowly removes waste and excess fluid over an extended period, preventing rapid fluid shifts. The document then discusses the different modes of CRRT, including continuous venovenous hemofiltration, hemodialysis, and hemodiafiltration. It covers the principles, processes, equipment, and nursing management of CRRT.