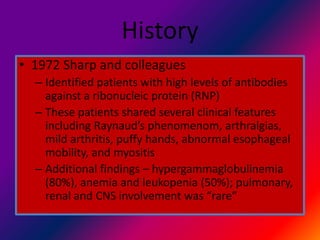
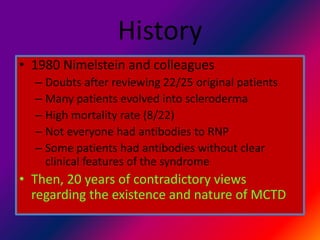
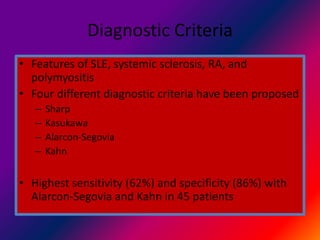
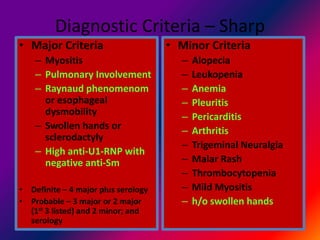
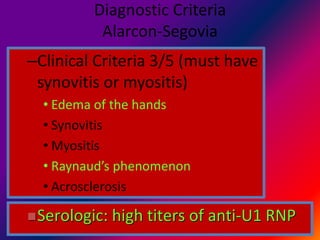
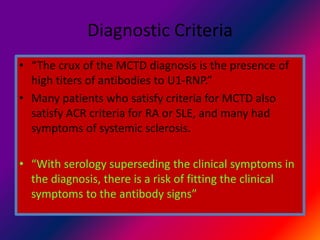
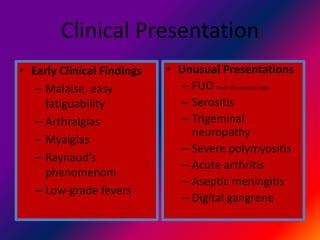
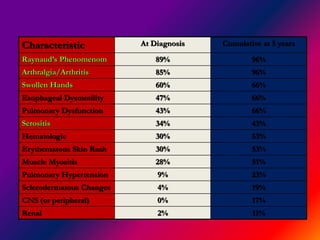
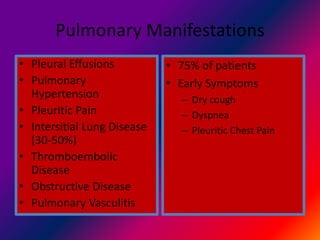
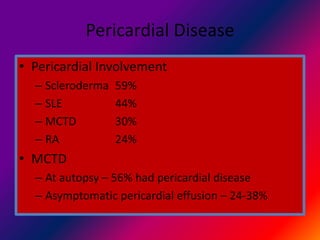
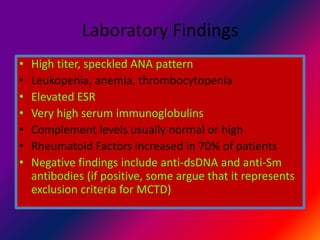
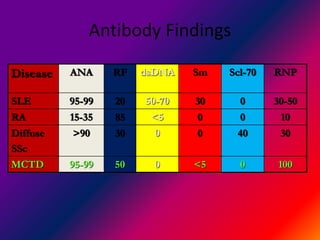
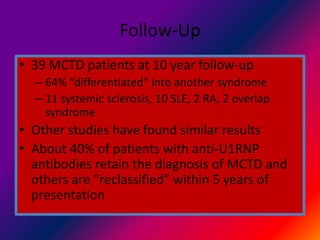
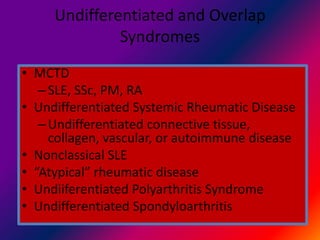
Mixed connective tissue disease (MCTD) is a rare autoimmune disorder with features of lupus, scleroderma, rheumatoid arthritis, and polymyositis. It is characterized by high levels of antibodies against ribonucleic proteins. Diagnostic criteria require 3 of 5 clinical features plus positive serology. Over time, many patients evolve symptoms meeting criteria for other connective tissue diseases. Pulmonary, renal, and cardiac involvement are common complications. Prognosis depends on degree of organ involvement, with 5-year mortality of 8-19% reported.