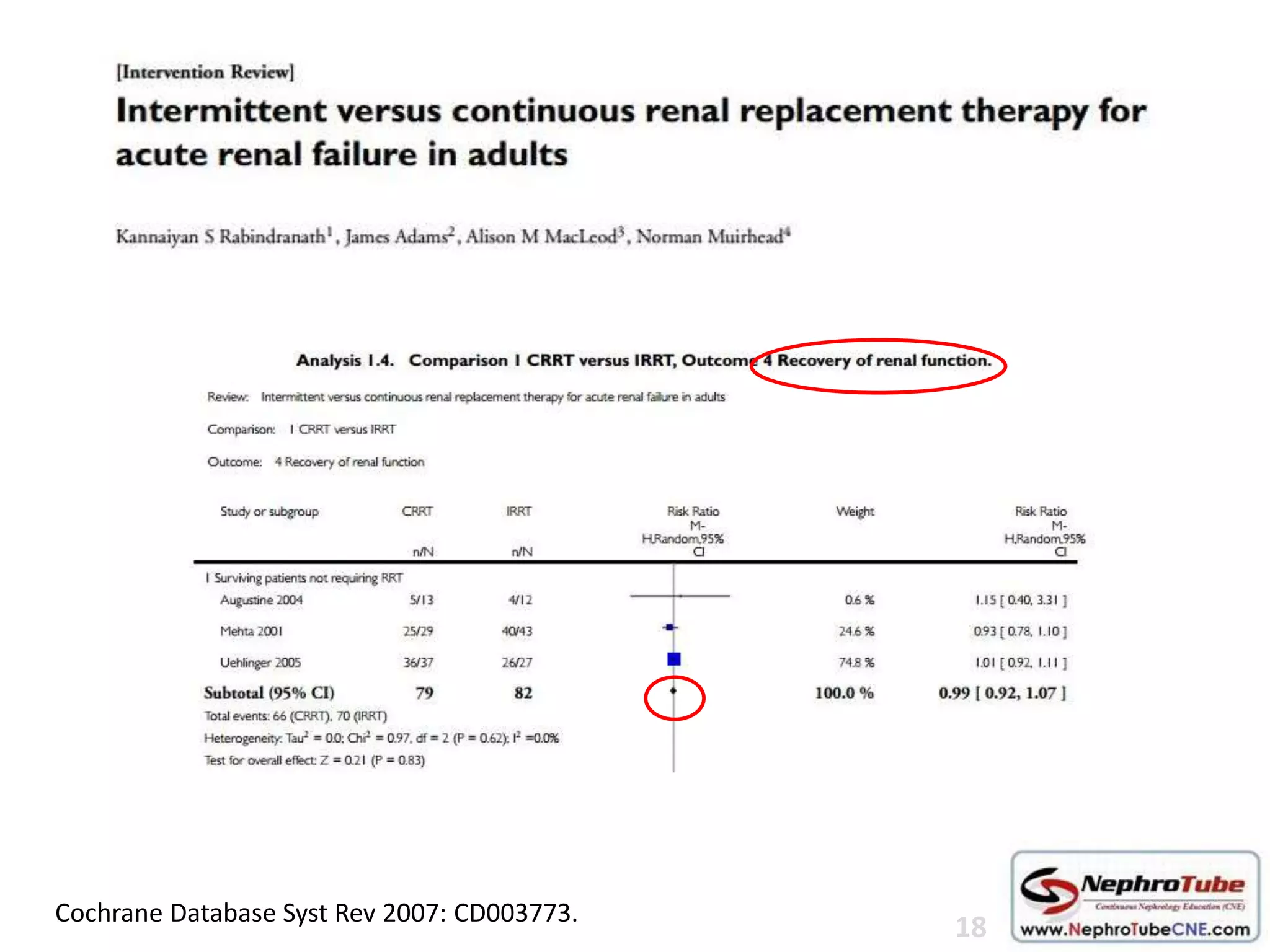
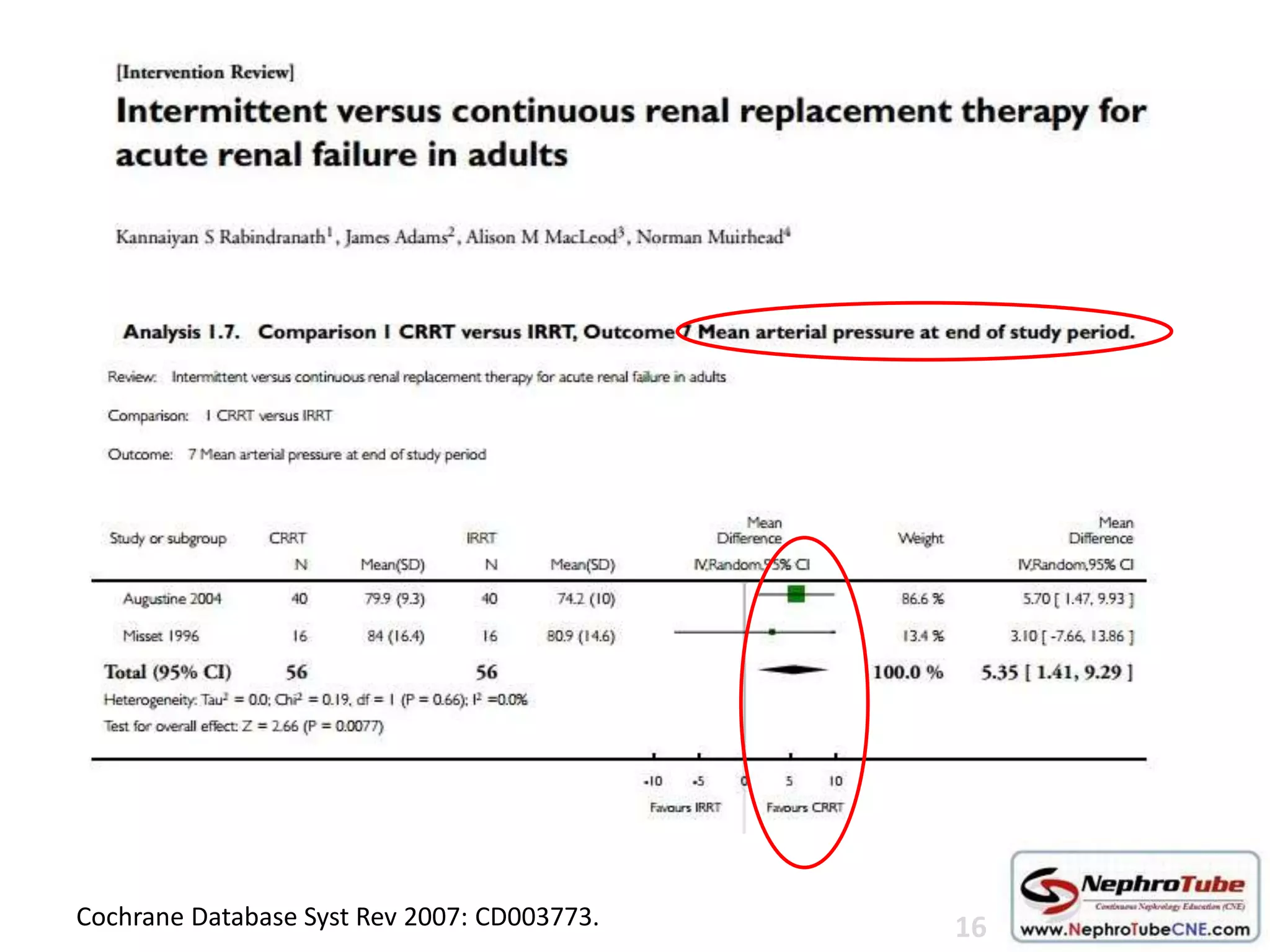
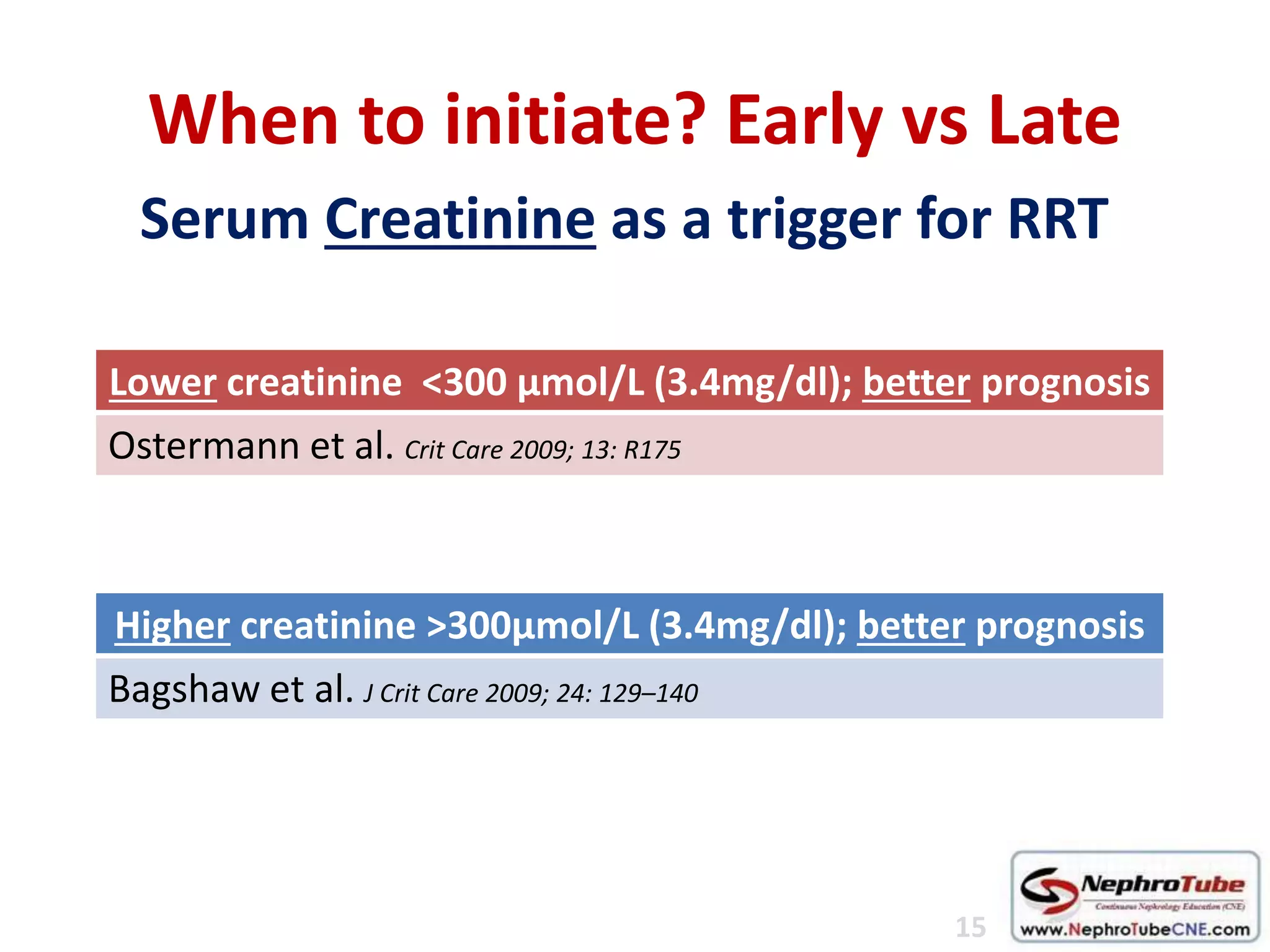
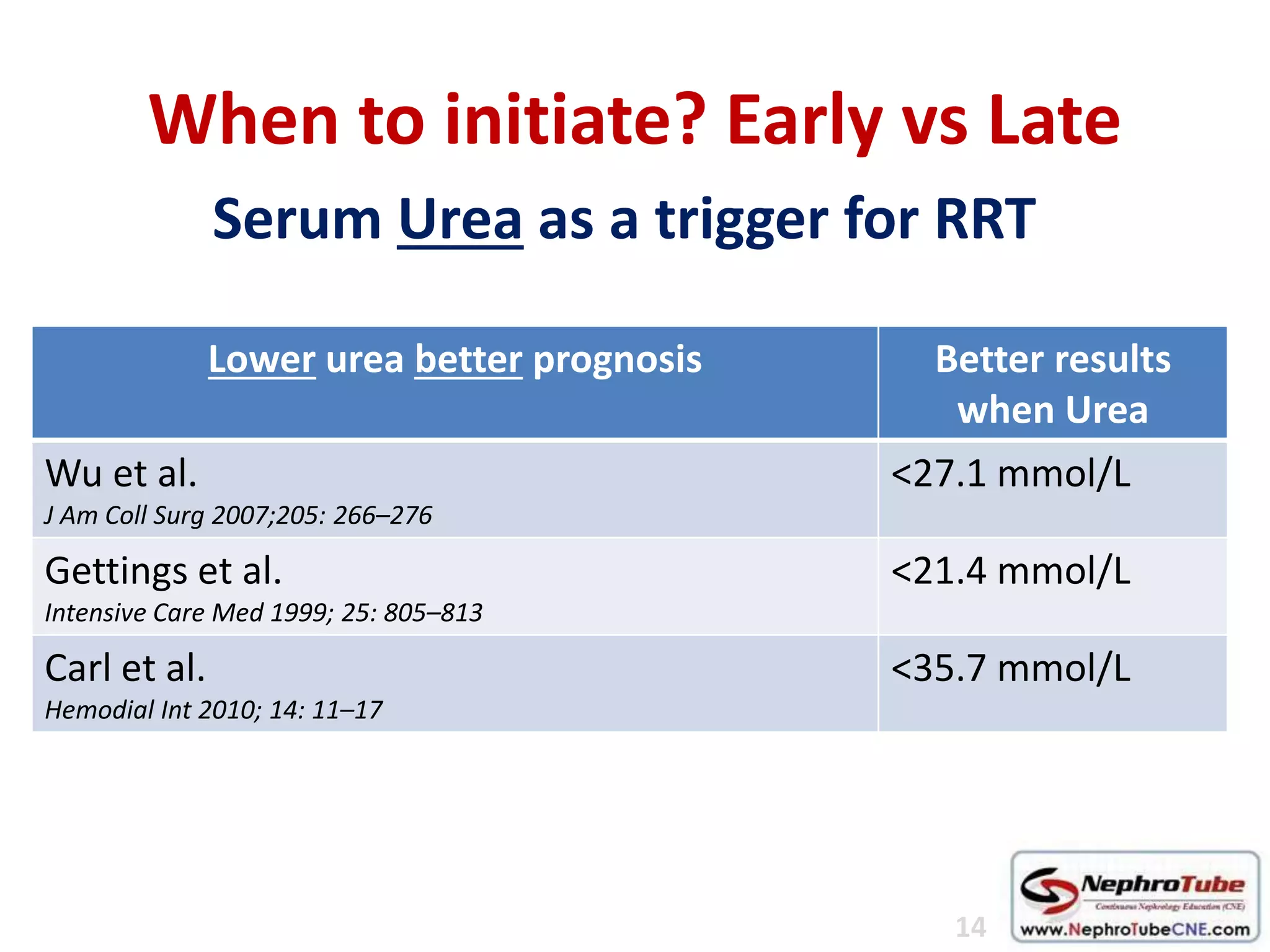
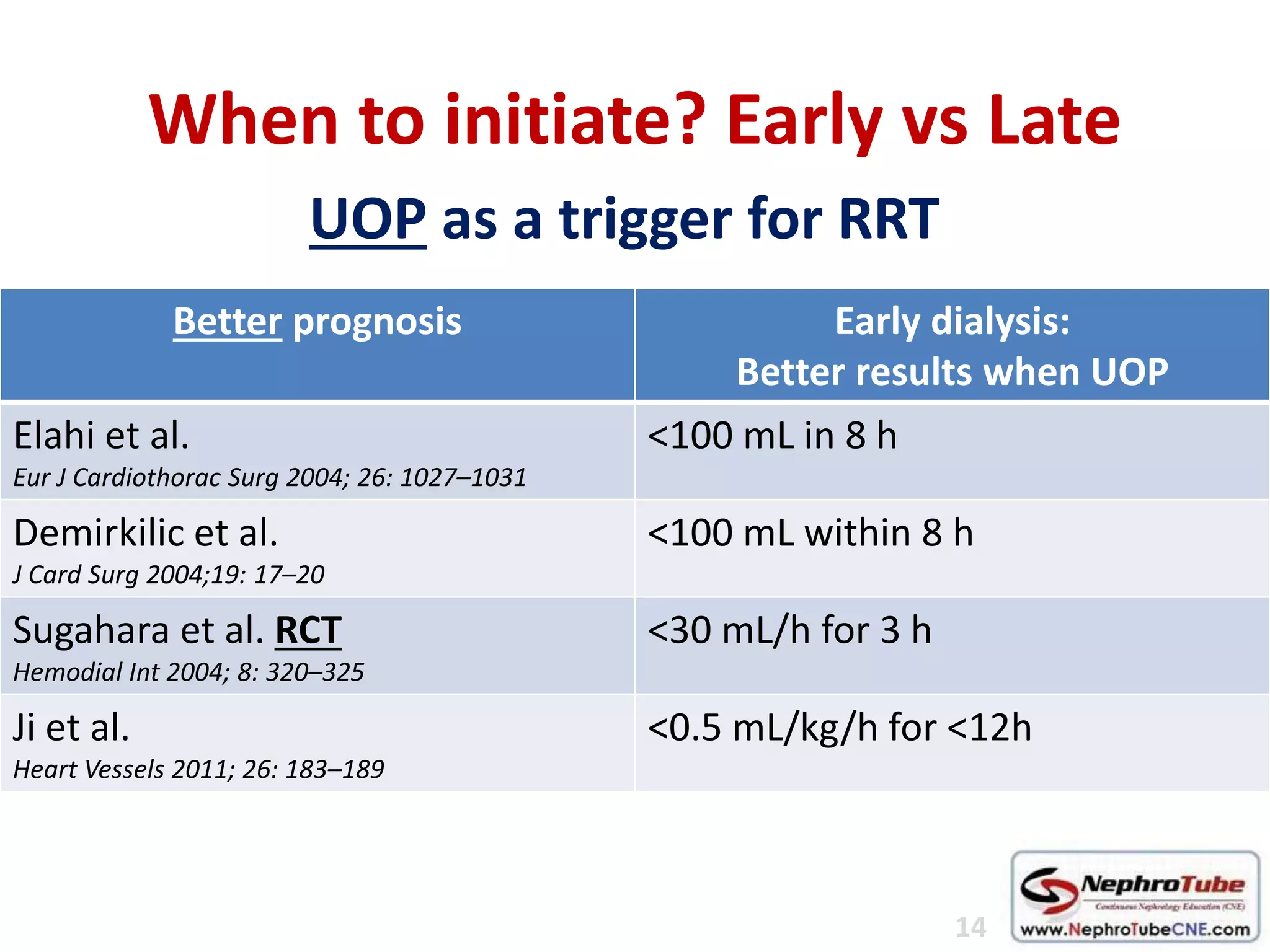
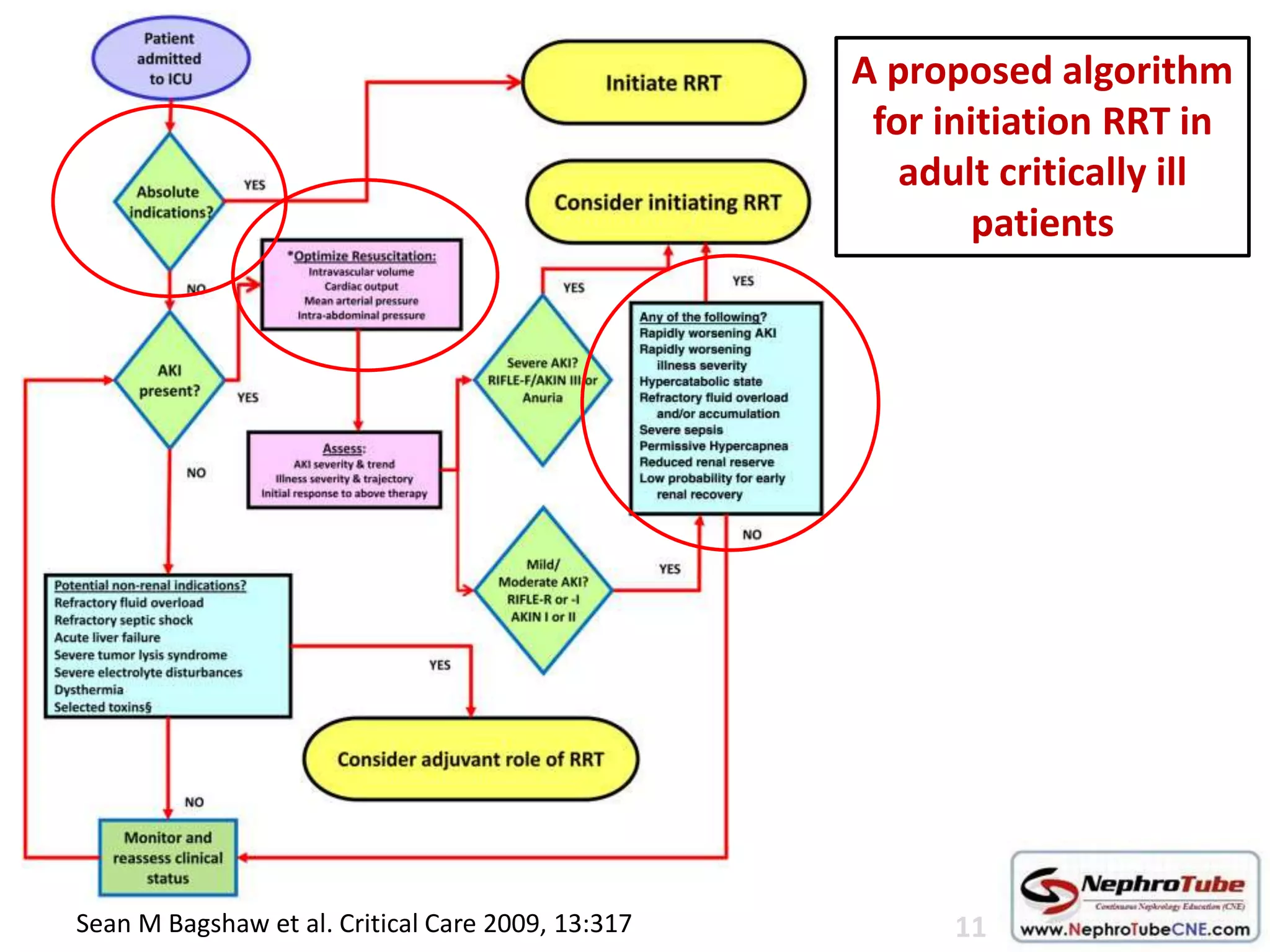
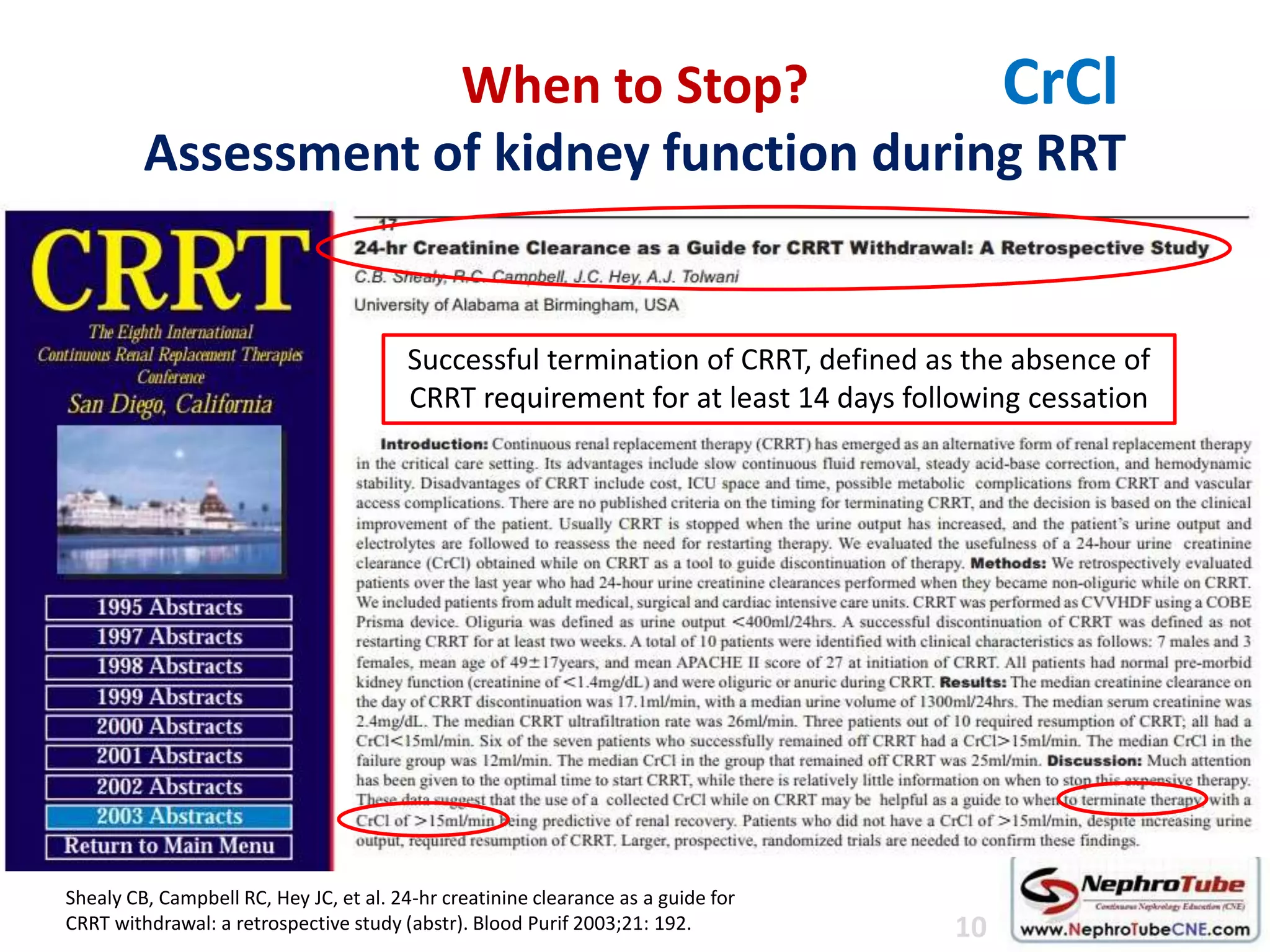
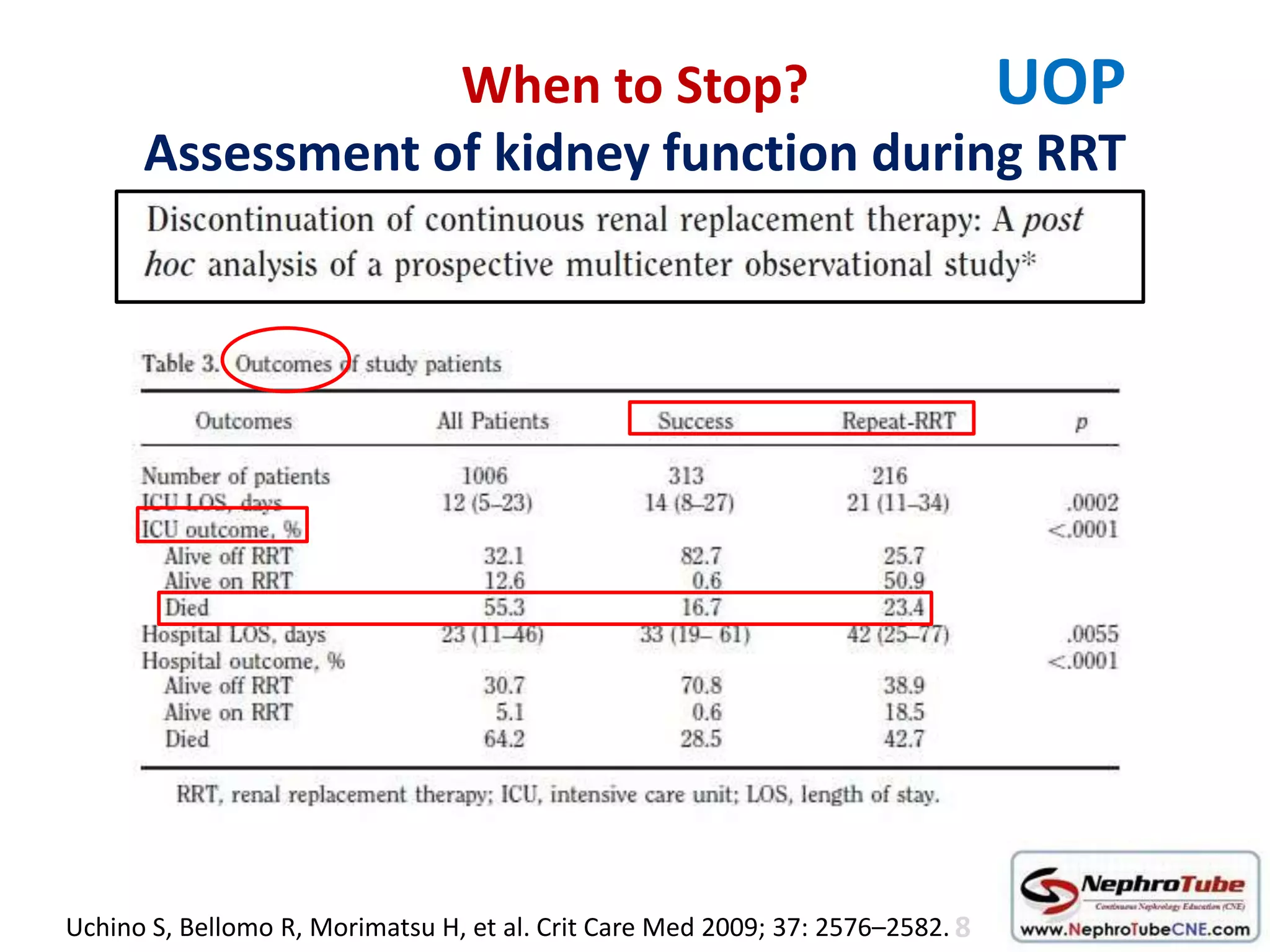
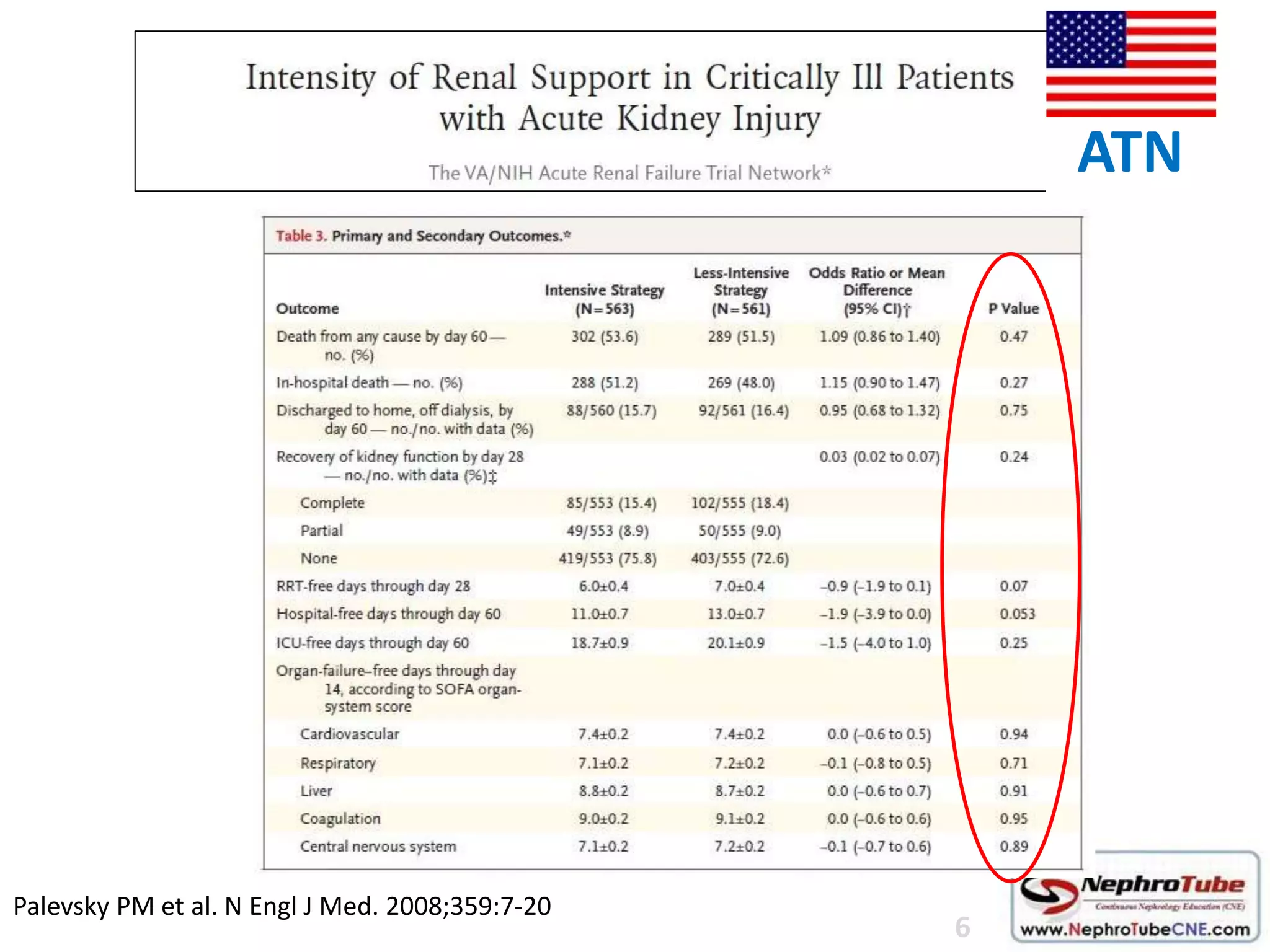
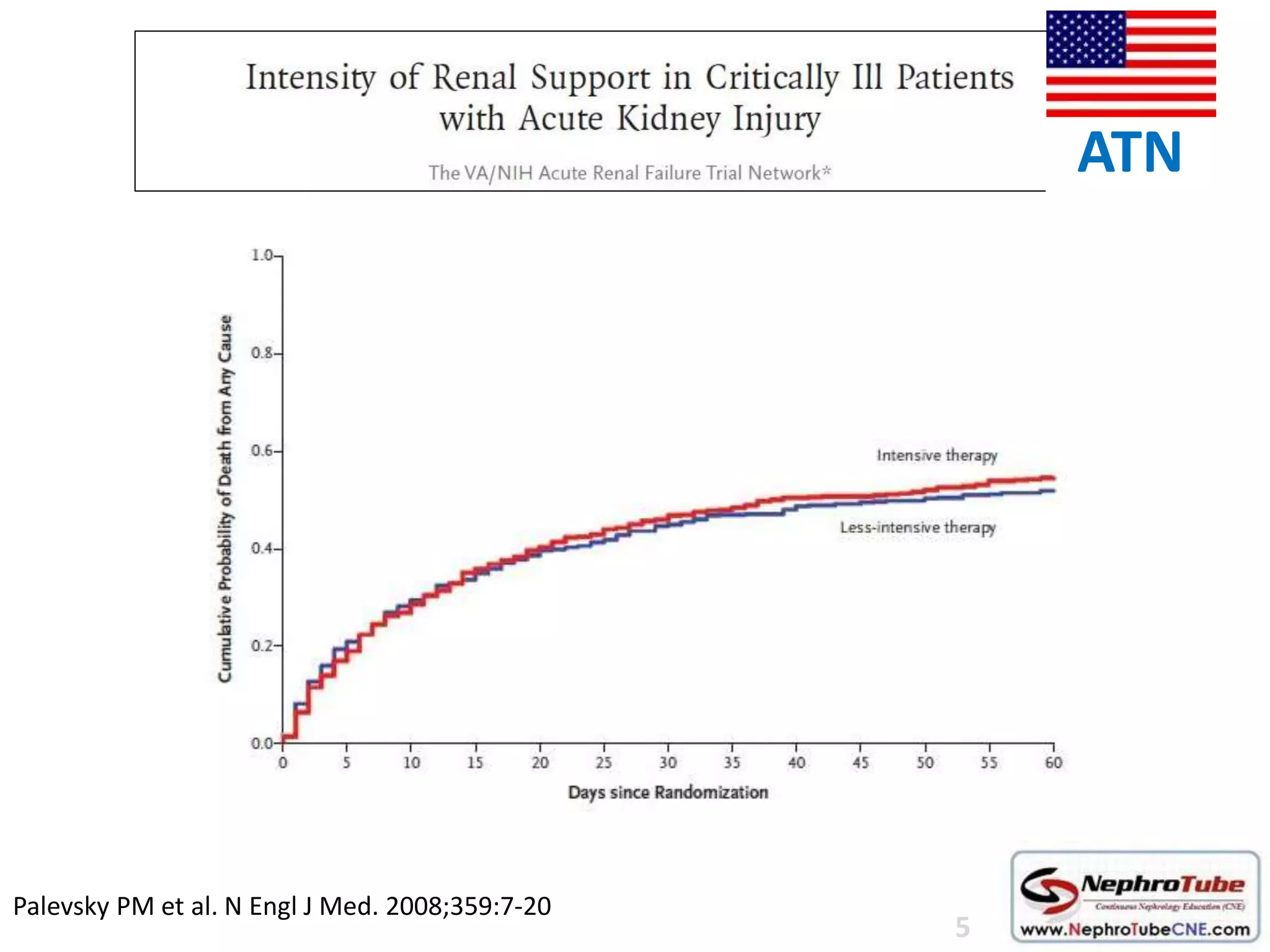
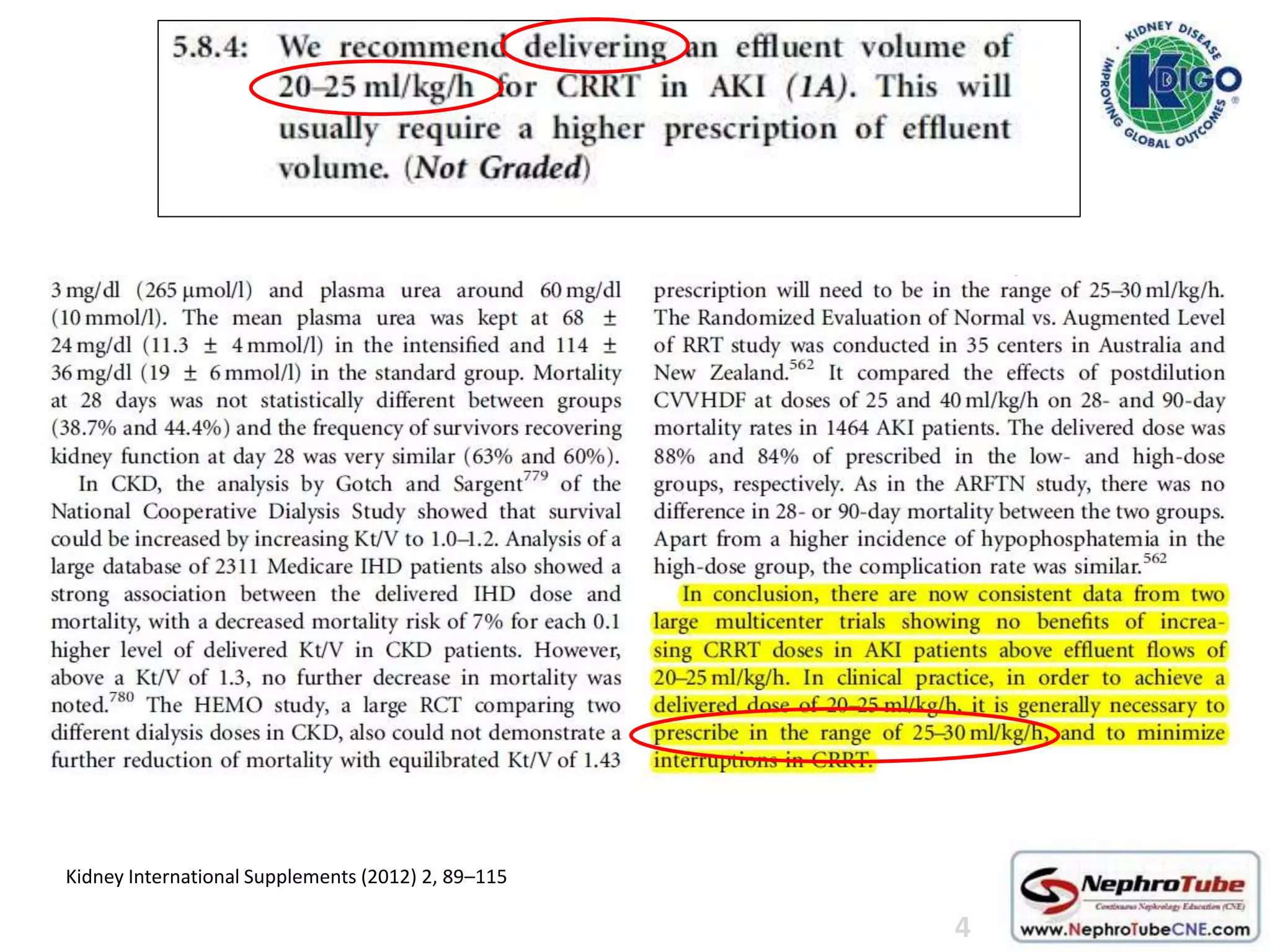
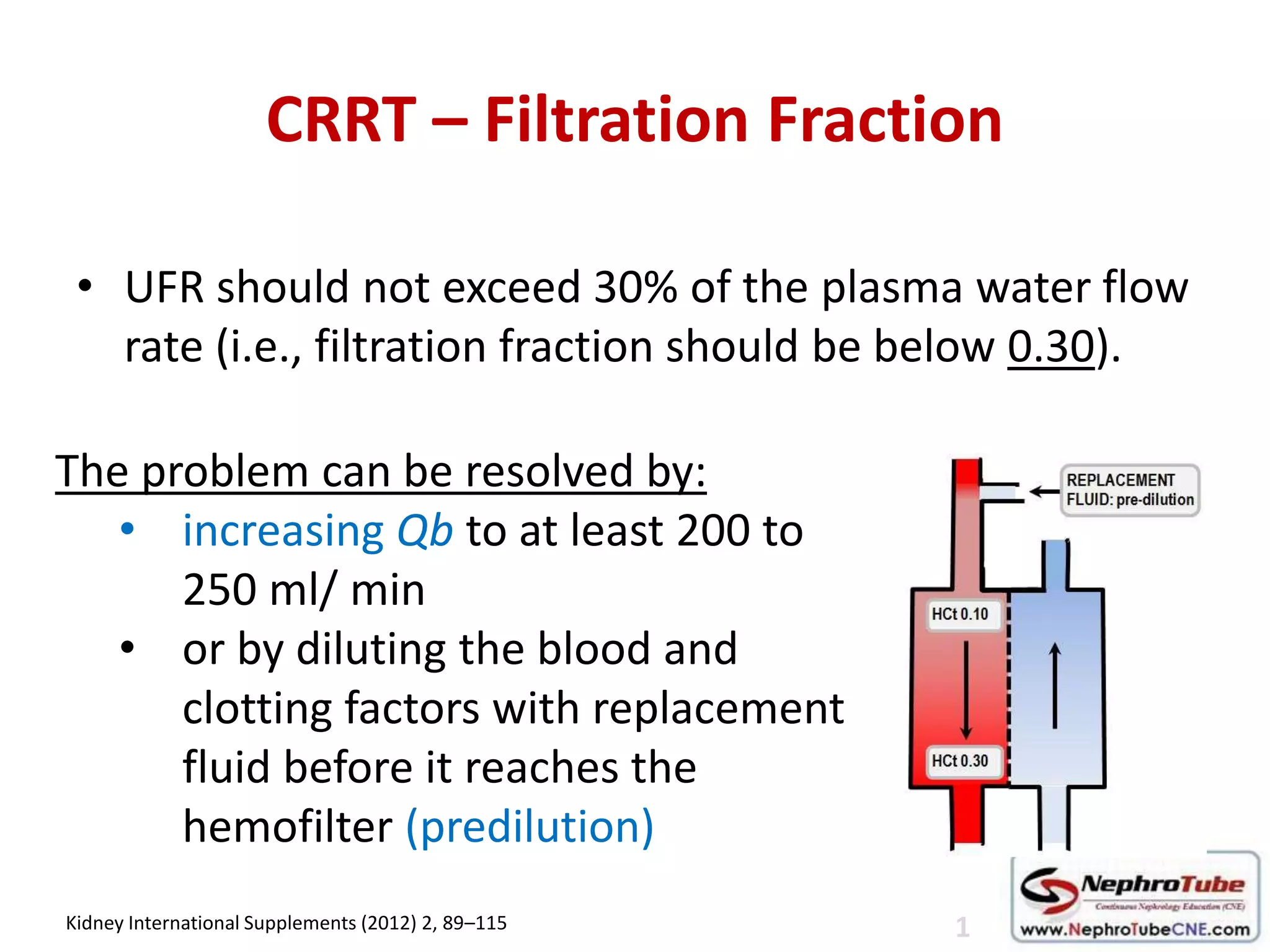
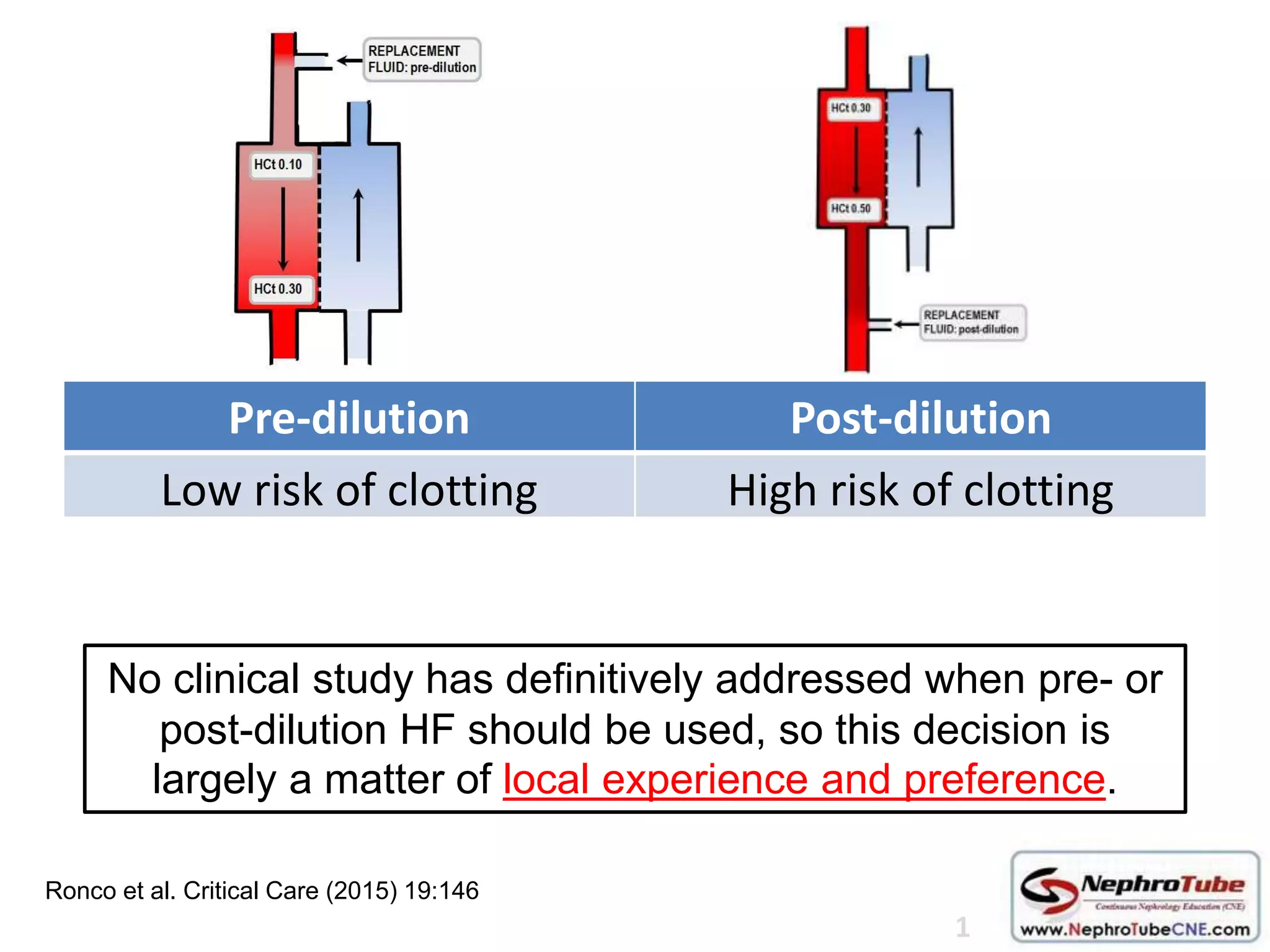
The document discusses continuous renal replacement therapy (CRRT) in ICU patients with acute kidney injury (AKI), evaluating its efficacy, timing for initiation and cessation, and considerations for dosing. Key points include the preference for CRRT in hemodynamically unstable patients, the importance of early diagnosis and timely intervention, and specific criteria for when to start or stop renal replacement therapy. Additionally, it highlights the need for tailored approaches based on individual patient conditions and clinical contexts.