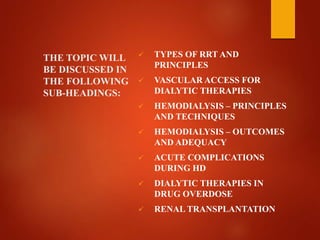
This document discusses various topics related to renal replacement therapy including:
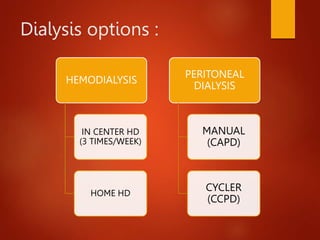
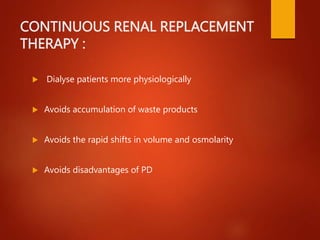
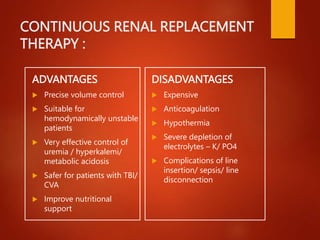
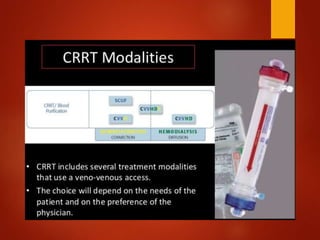
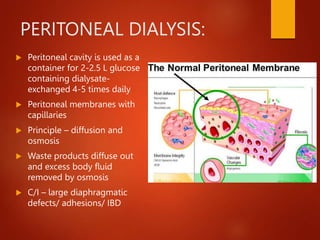
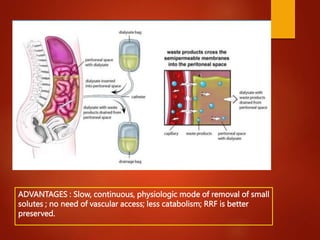
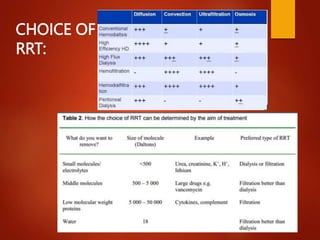
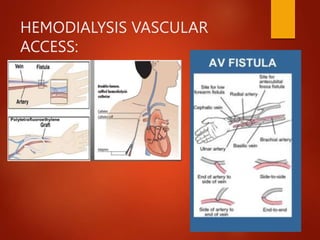
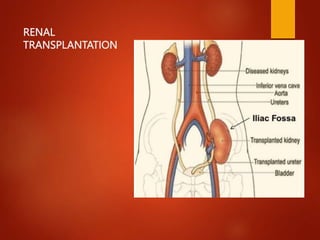
1. Types of renal replacement therapy such as hemodialysis, peritoneal dialysis, and renal transplantation.
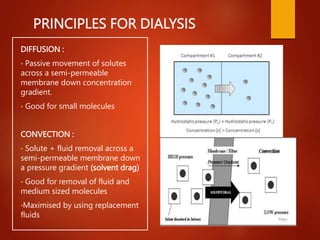
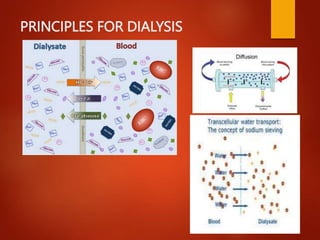
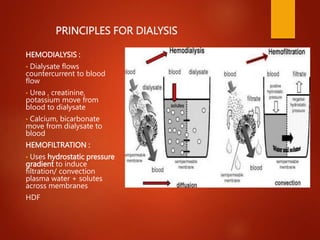
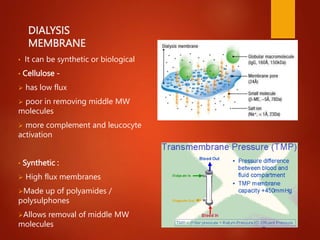
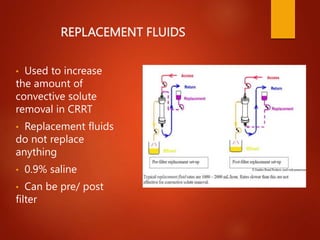
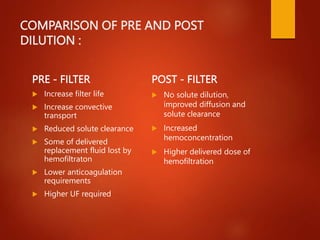
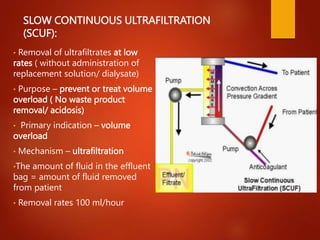
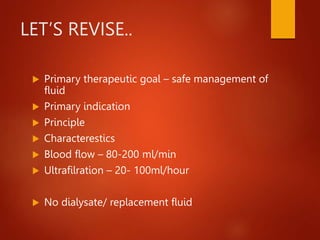
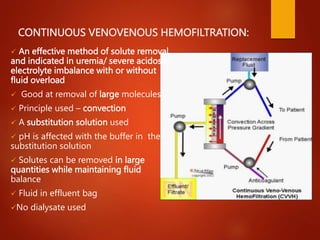
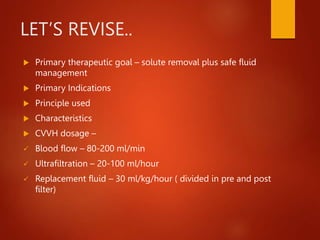
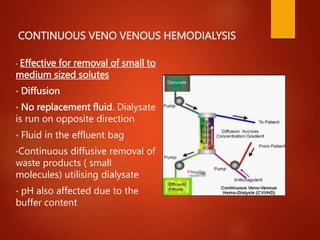
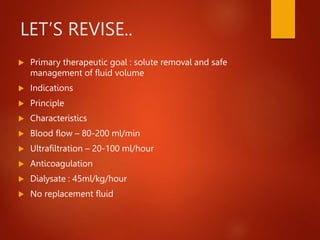
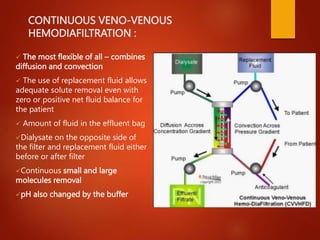
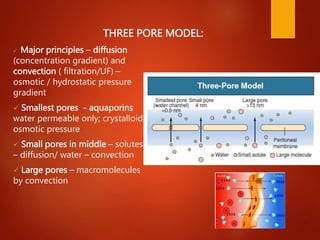
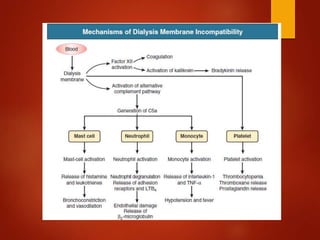
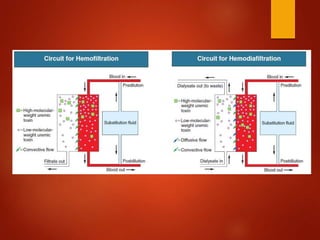
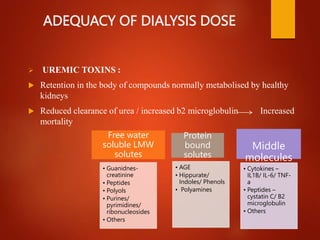
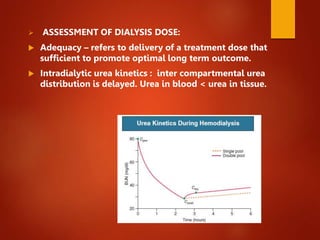
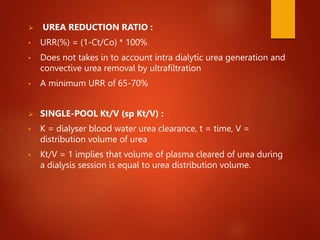
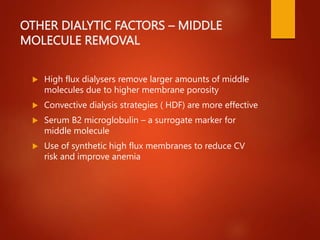
2. Principles of dialysis including diffusion, convection, and regional citrate anticoagulation.
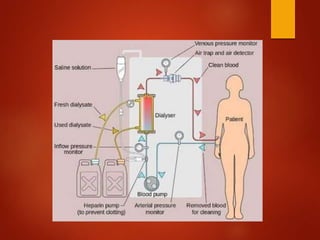
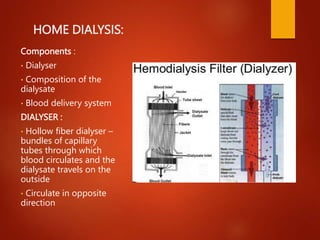
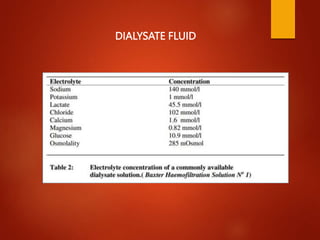
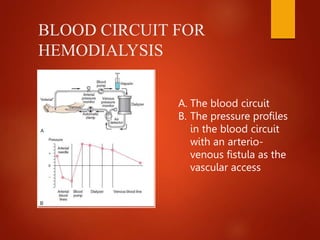
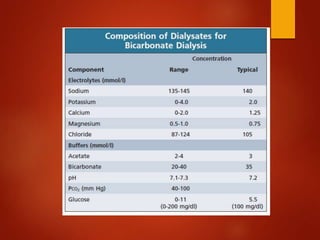
3. Components of home hemodialysis including the dialyzer, composition of dialysate, and blood delivery system.
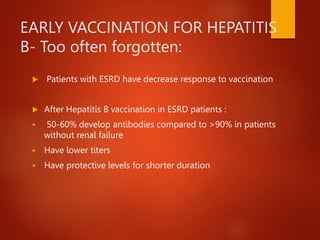
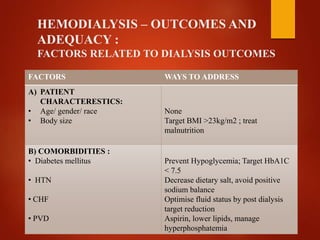
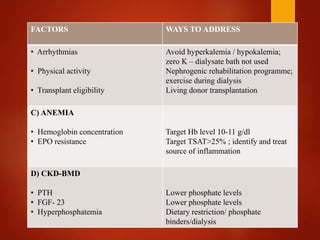
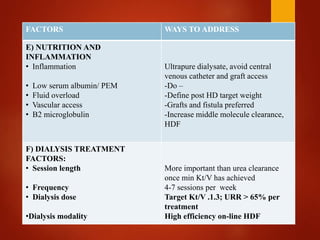
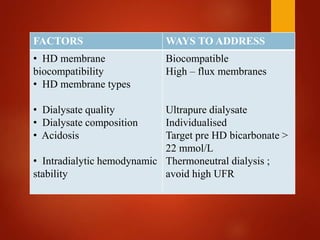
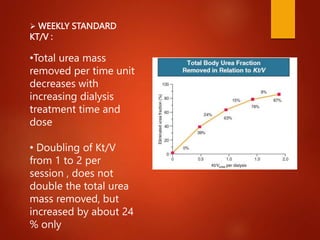
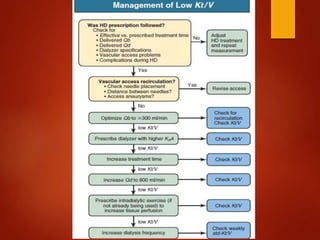
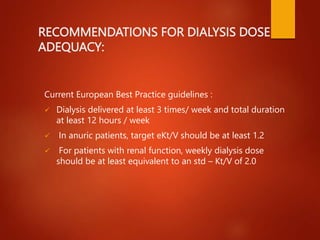
4. Factors that influence dialysis outcomes such as patient characteristics, comorbidities, nutrition, inflammation, and dialysis treatment factors.