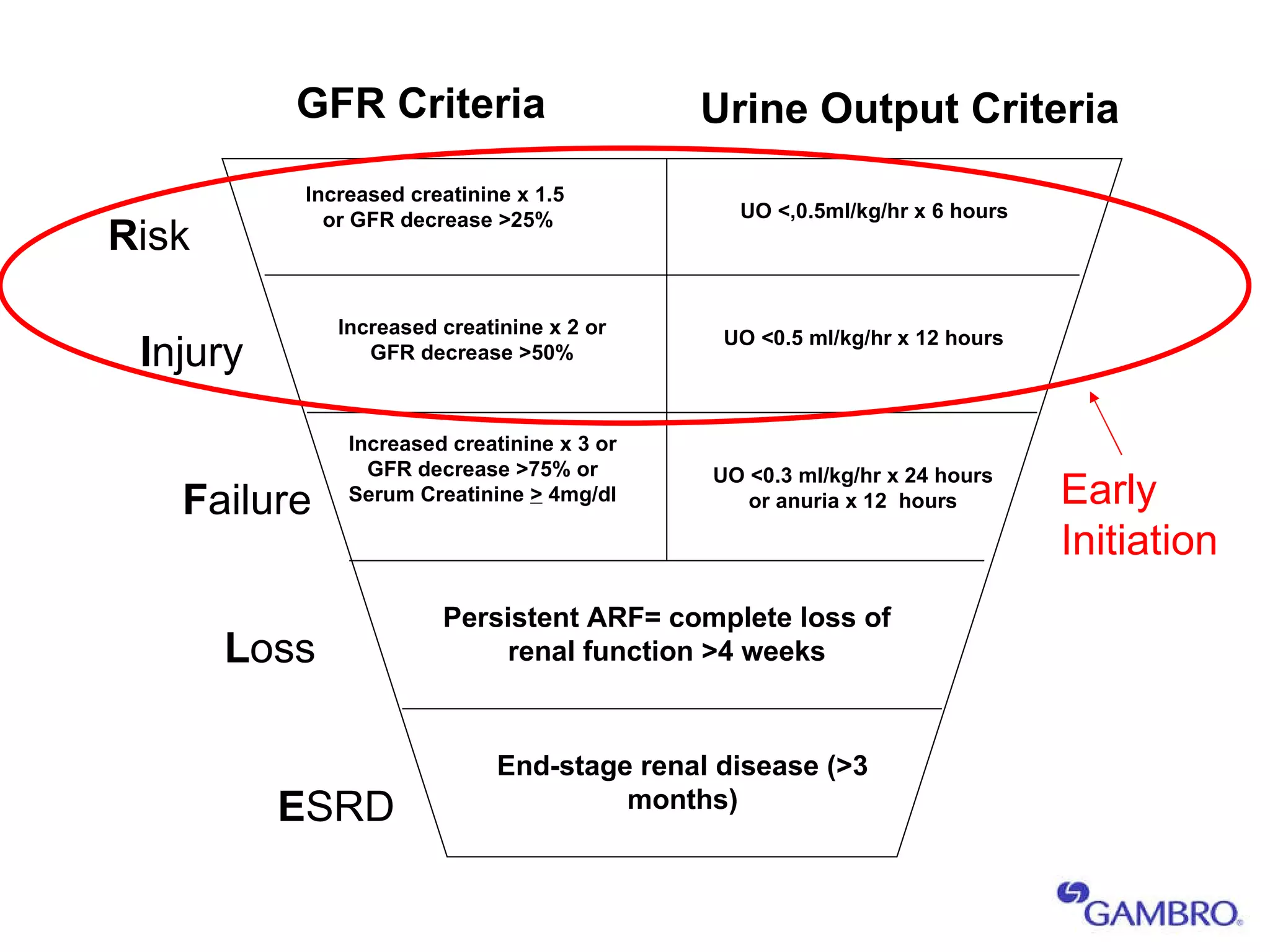
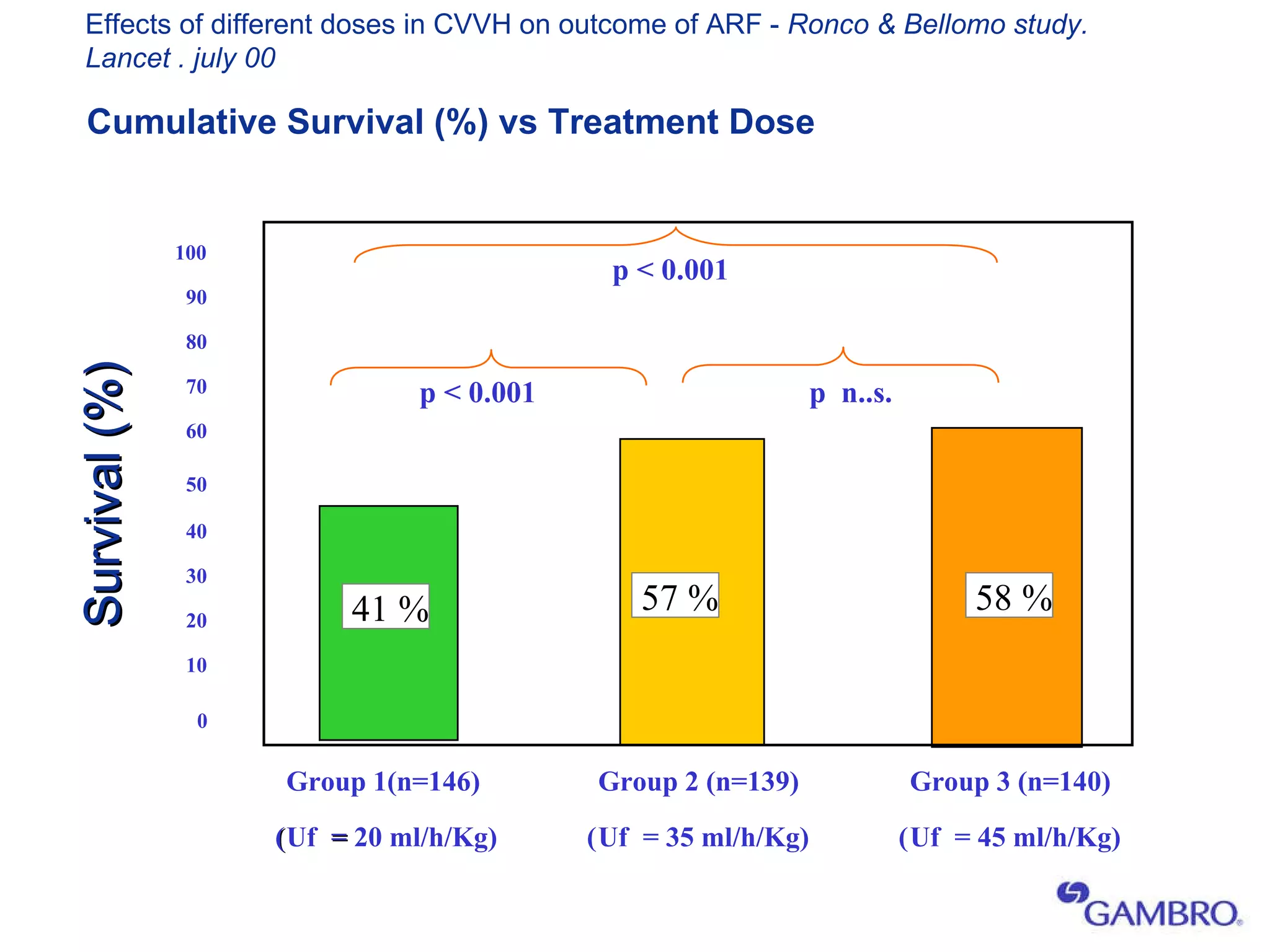
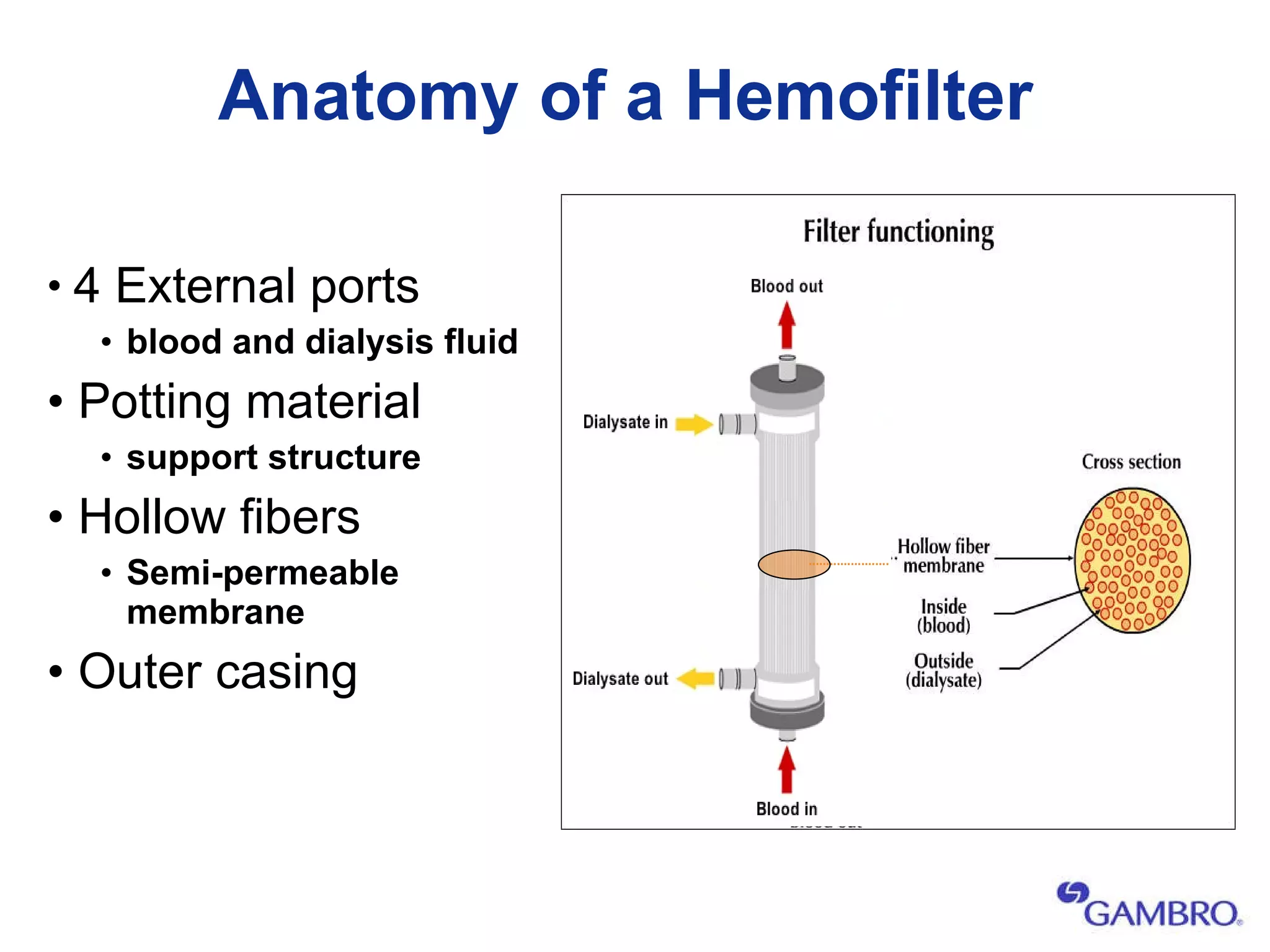
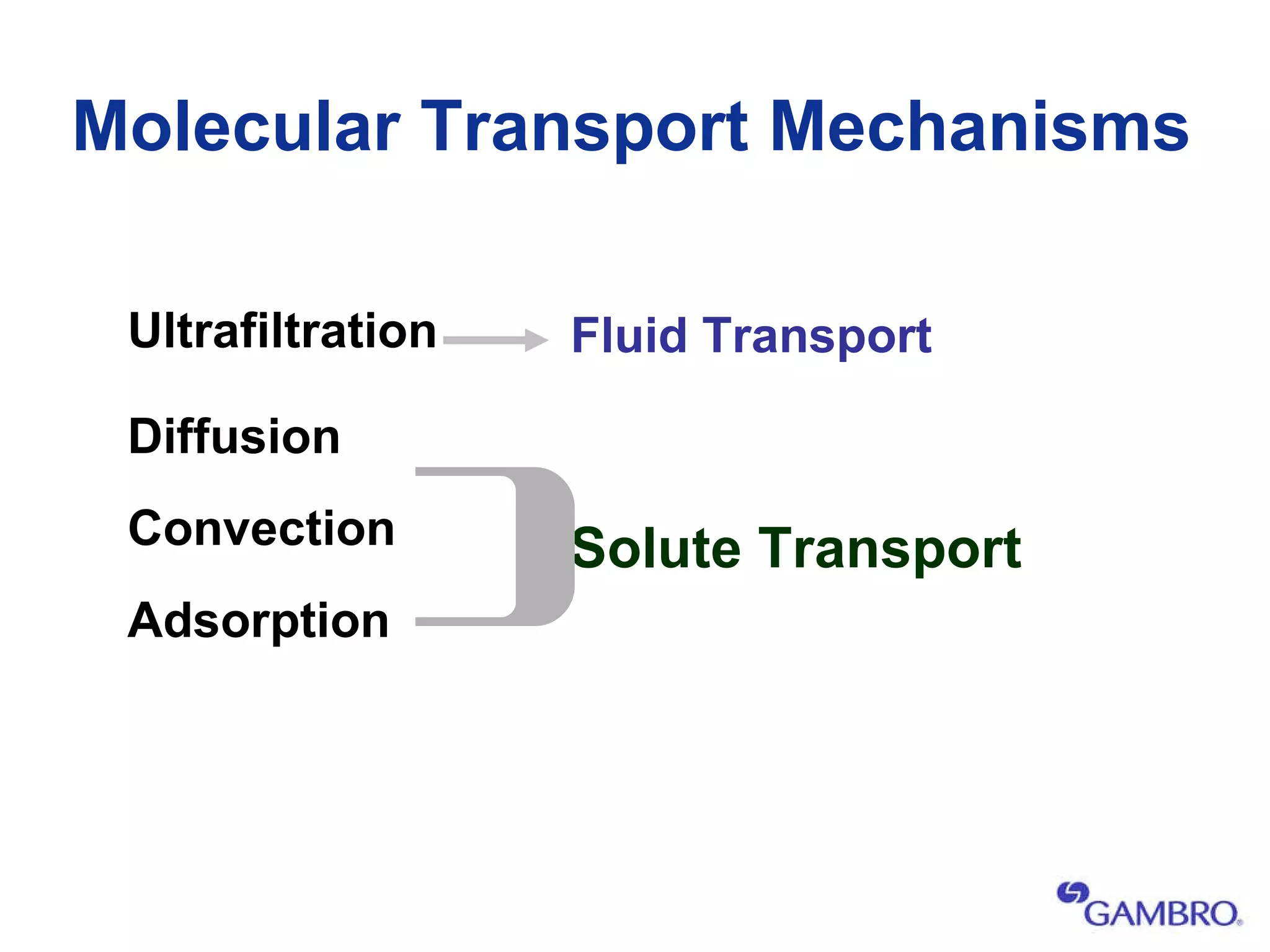
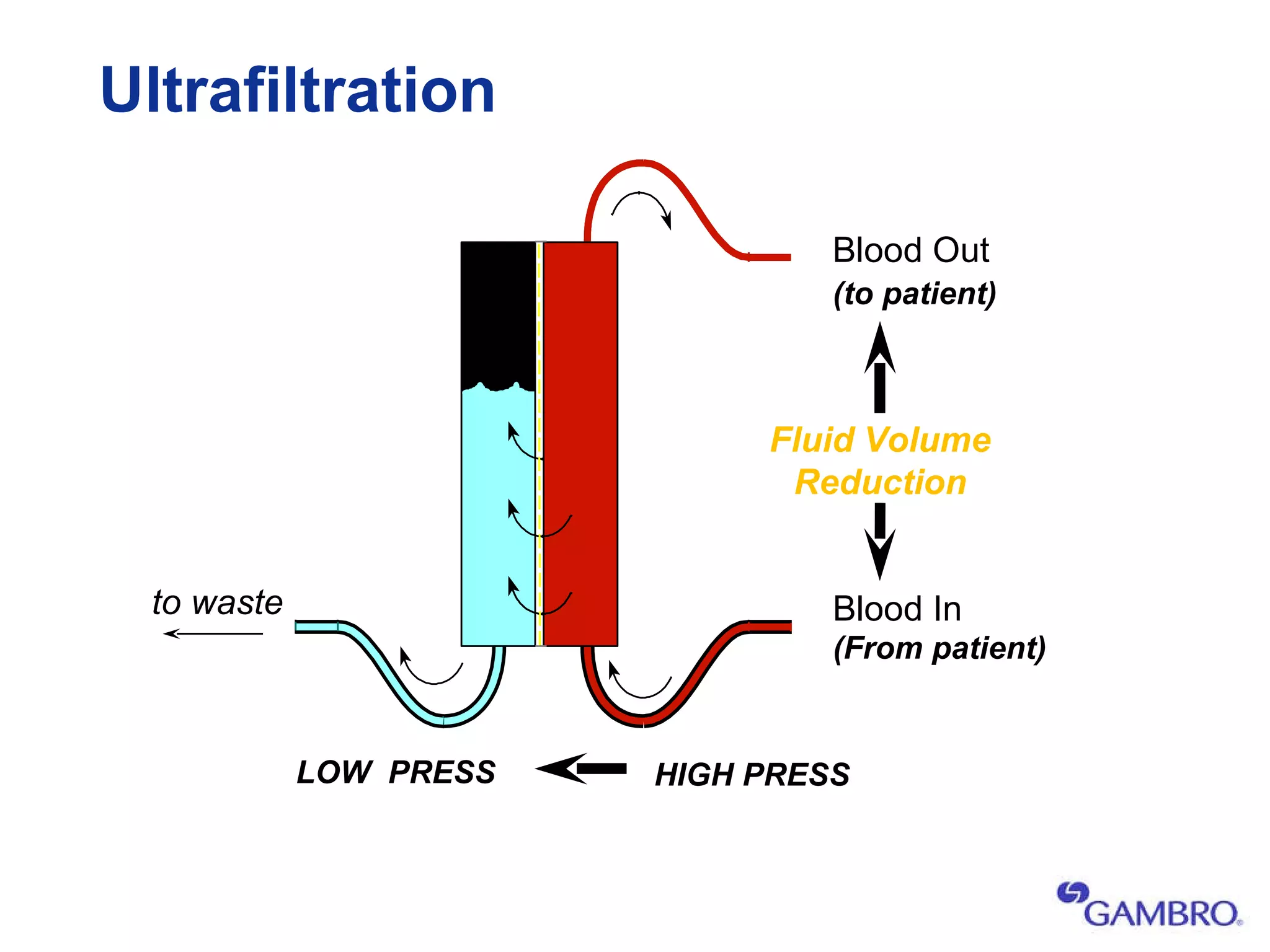
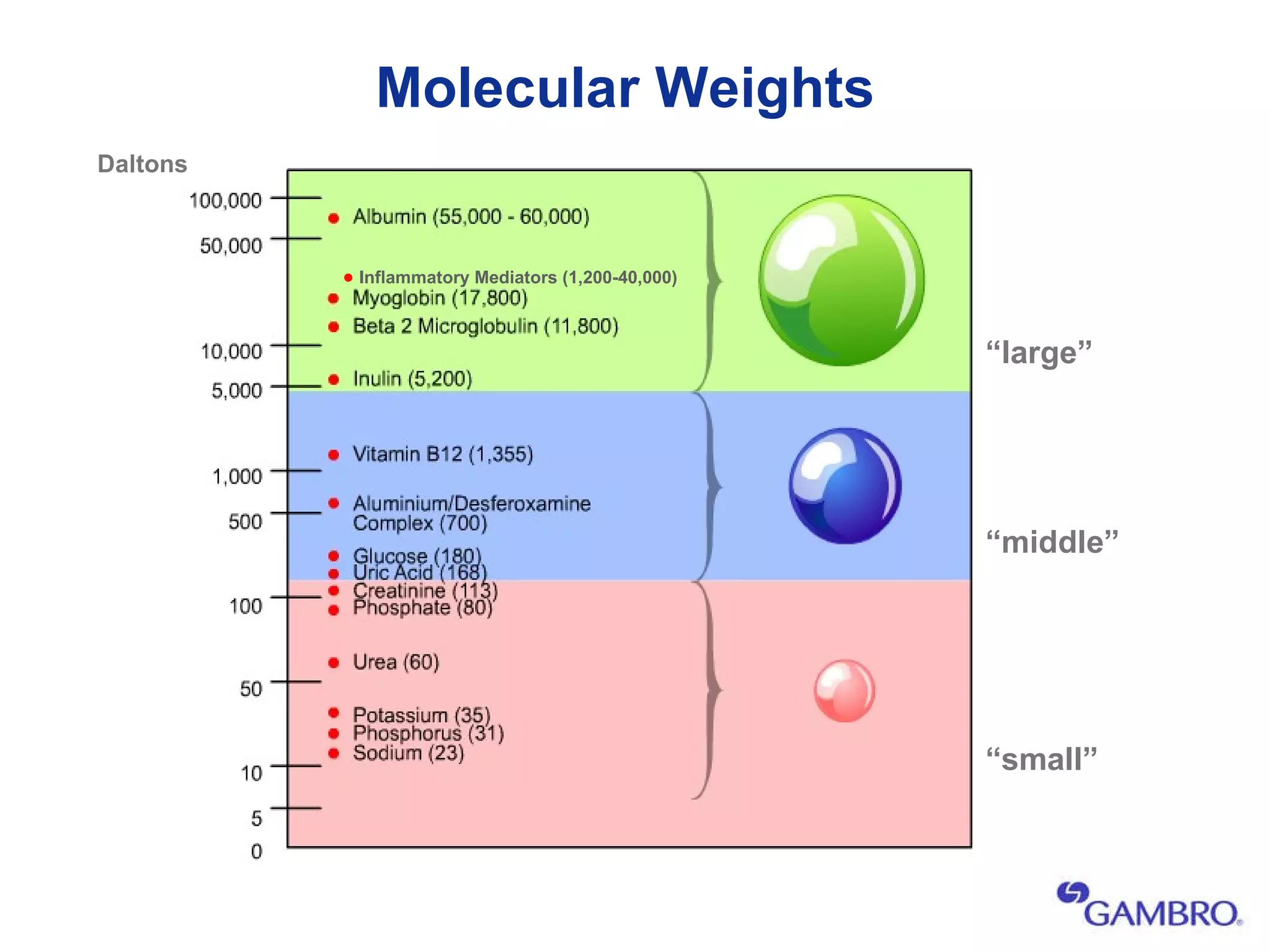
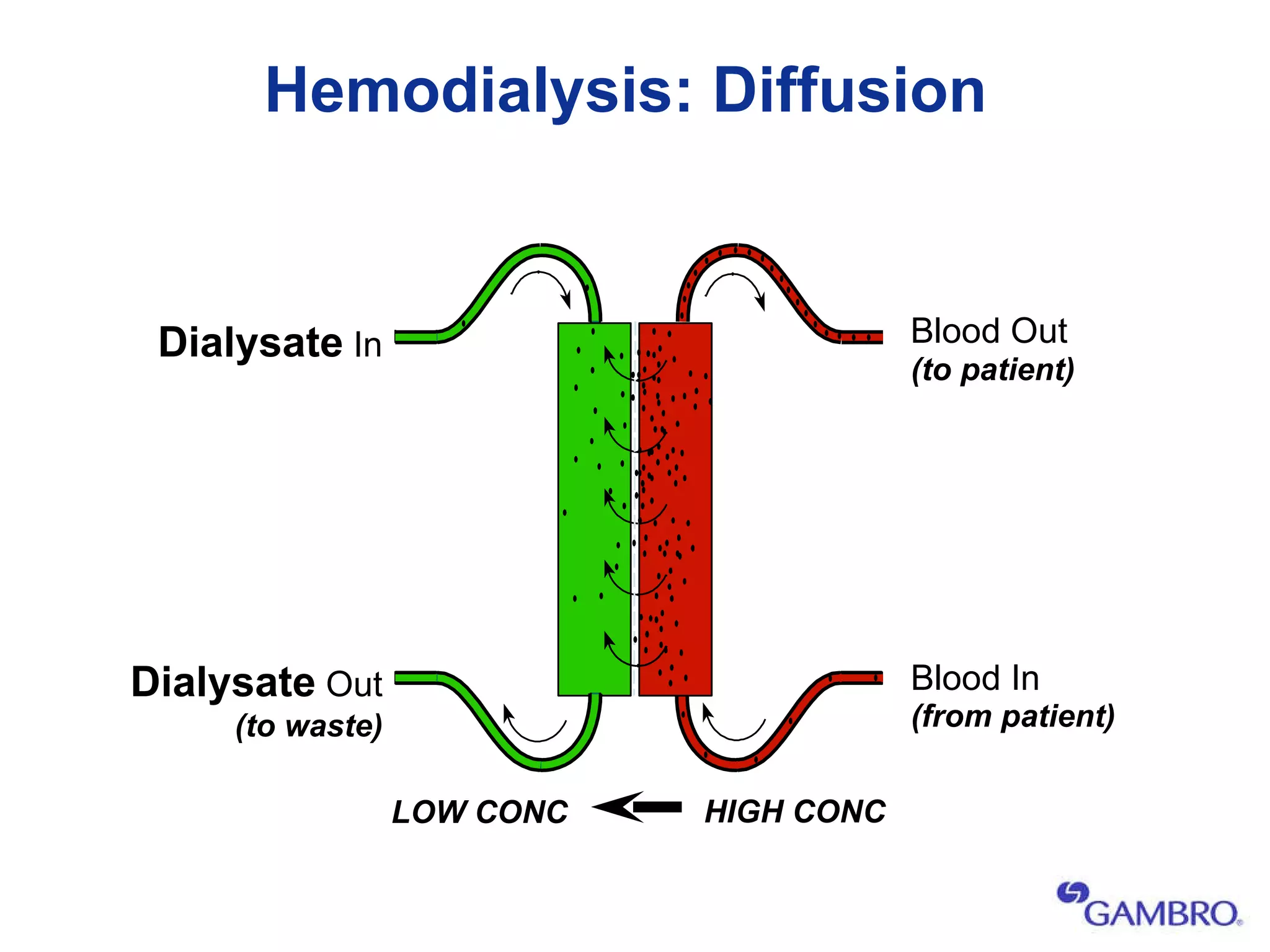
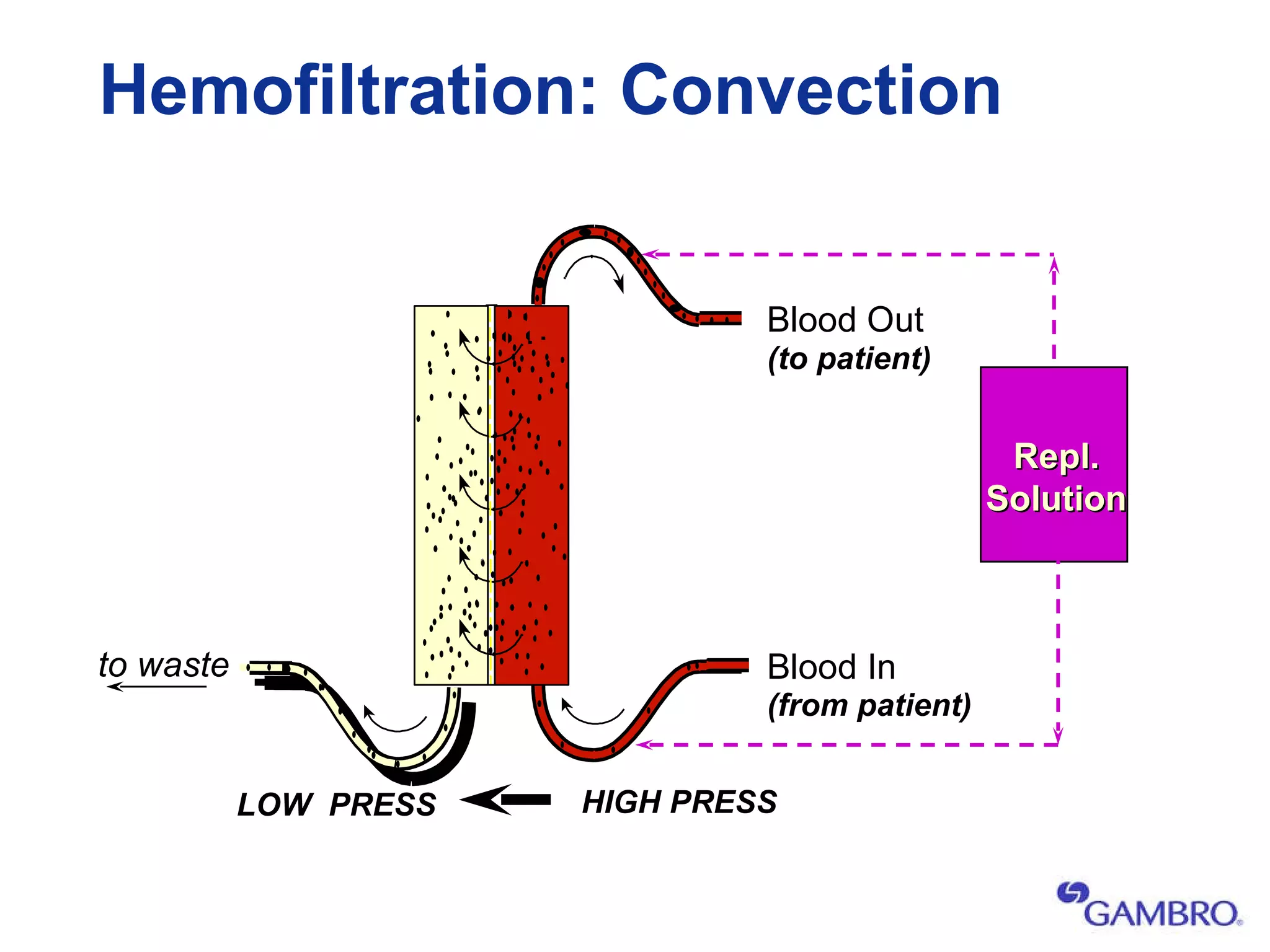
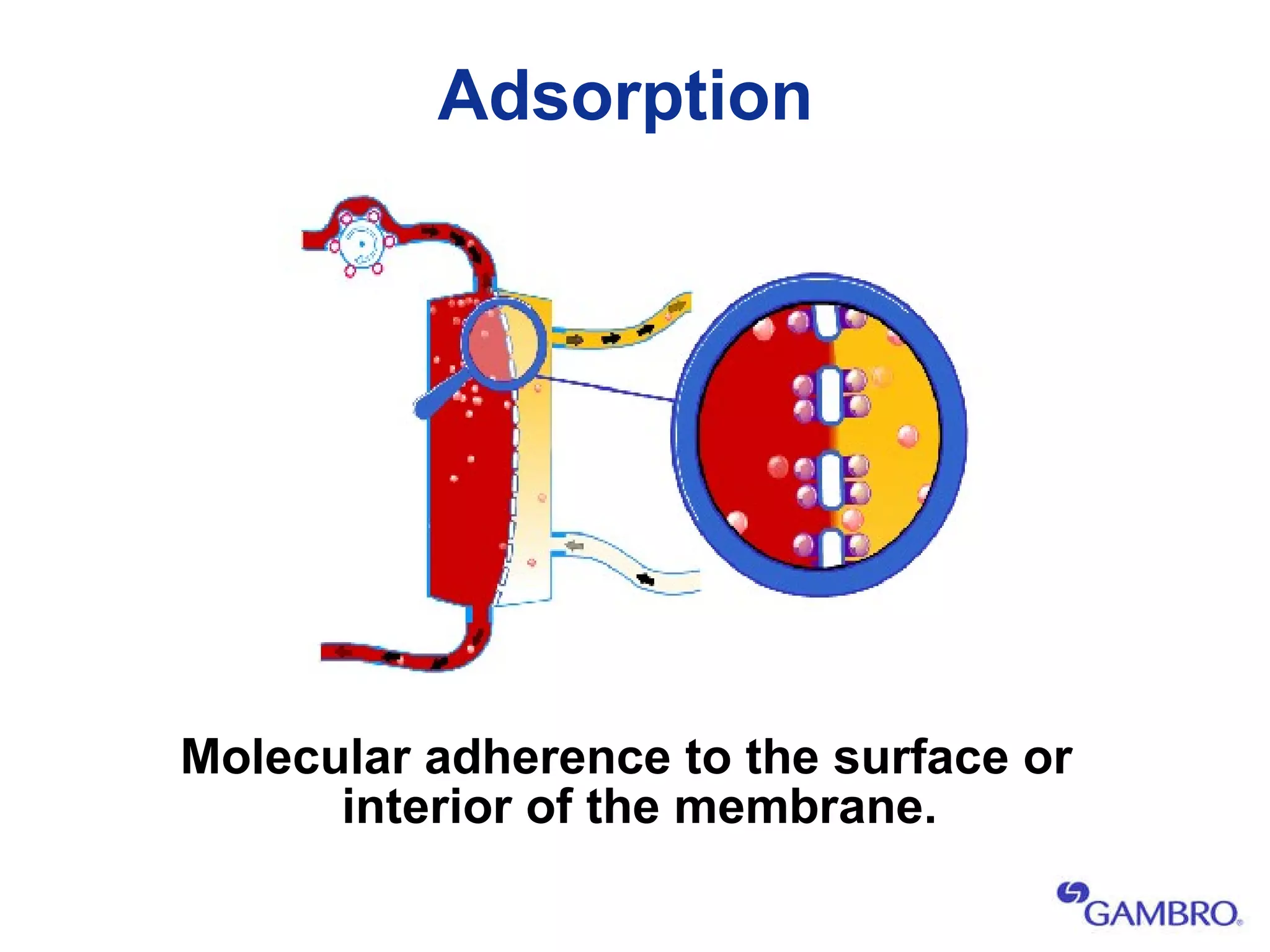
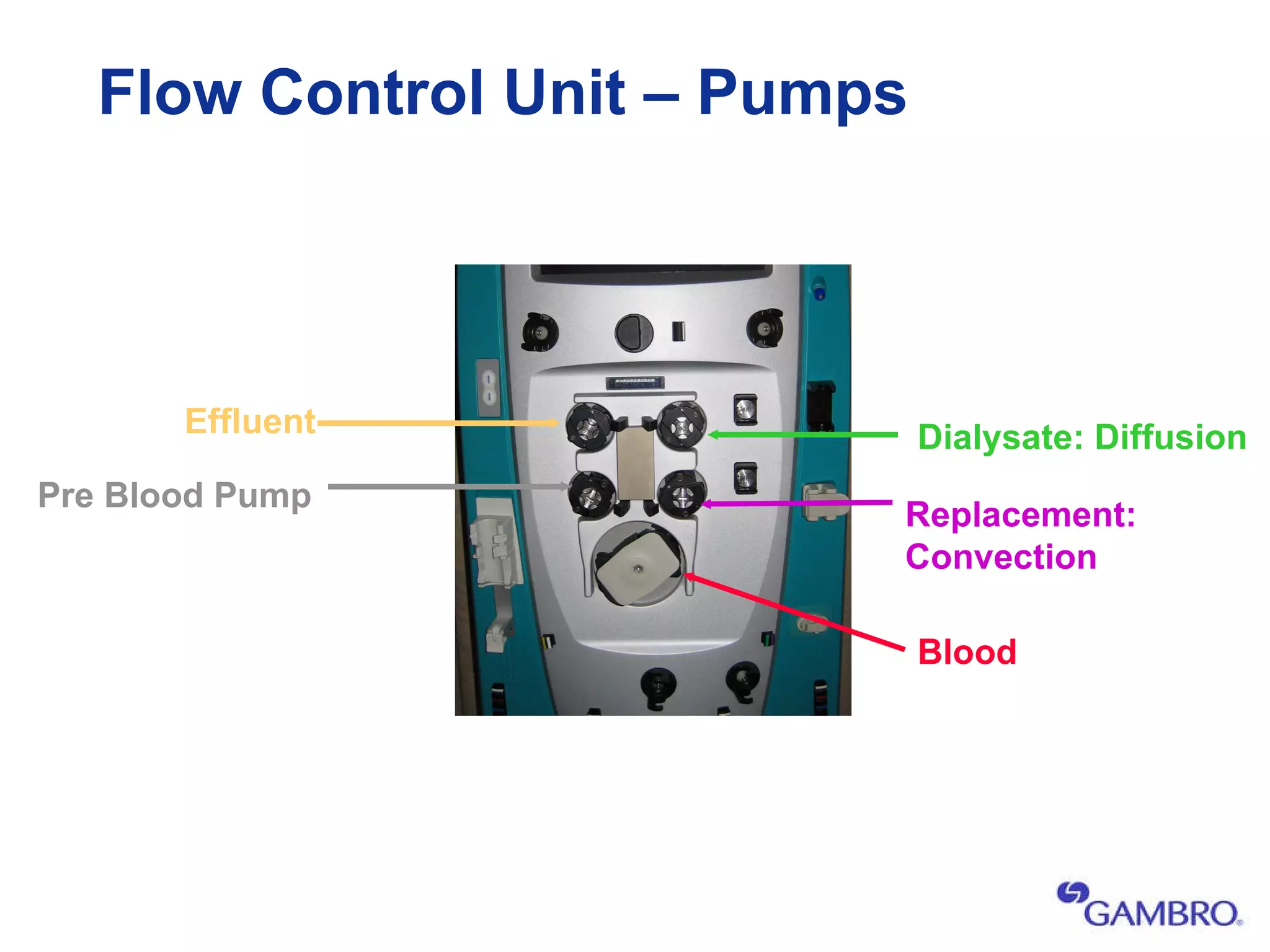
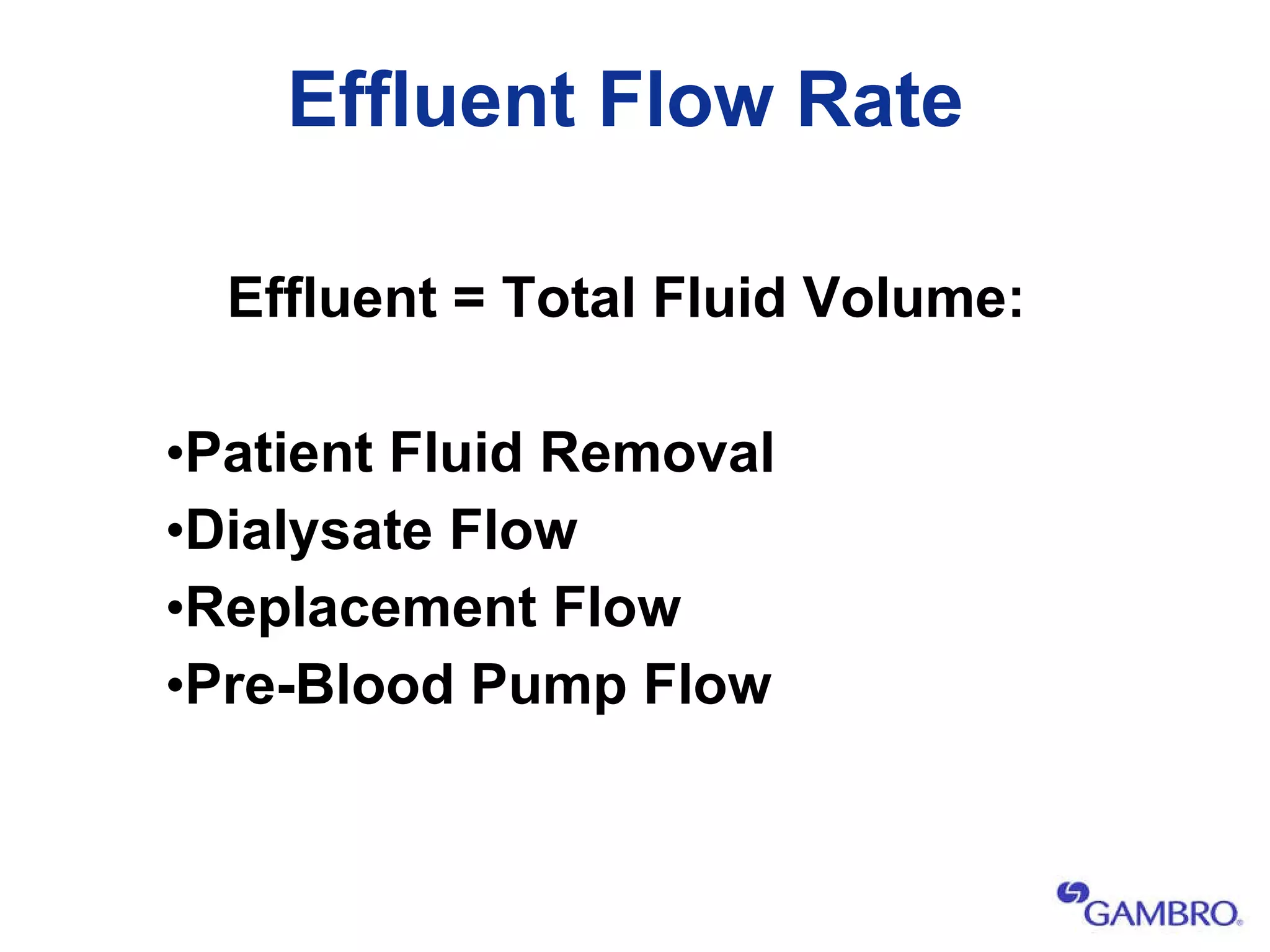
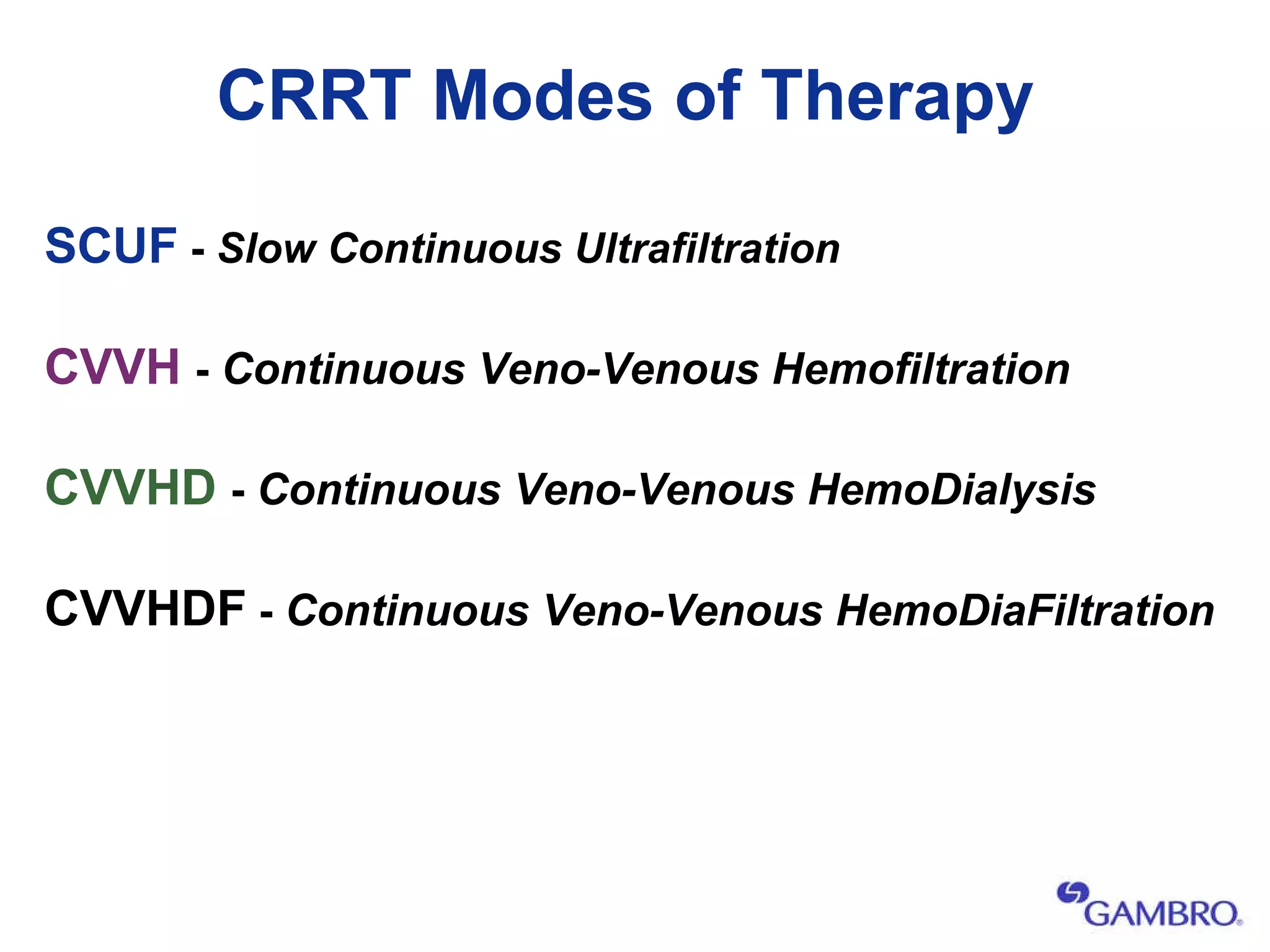
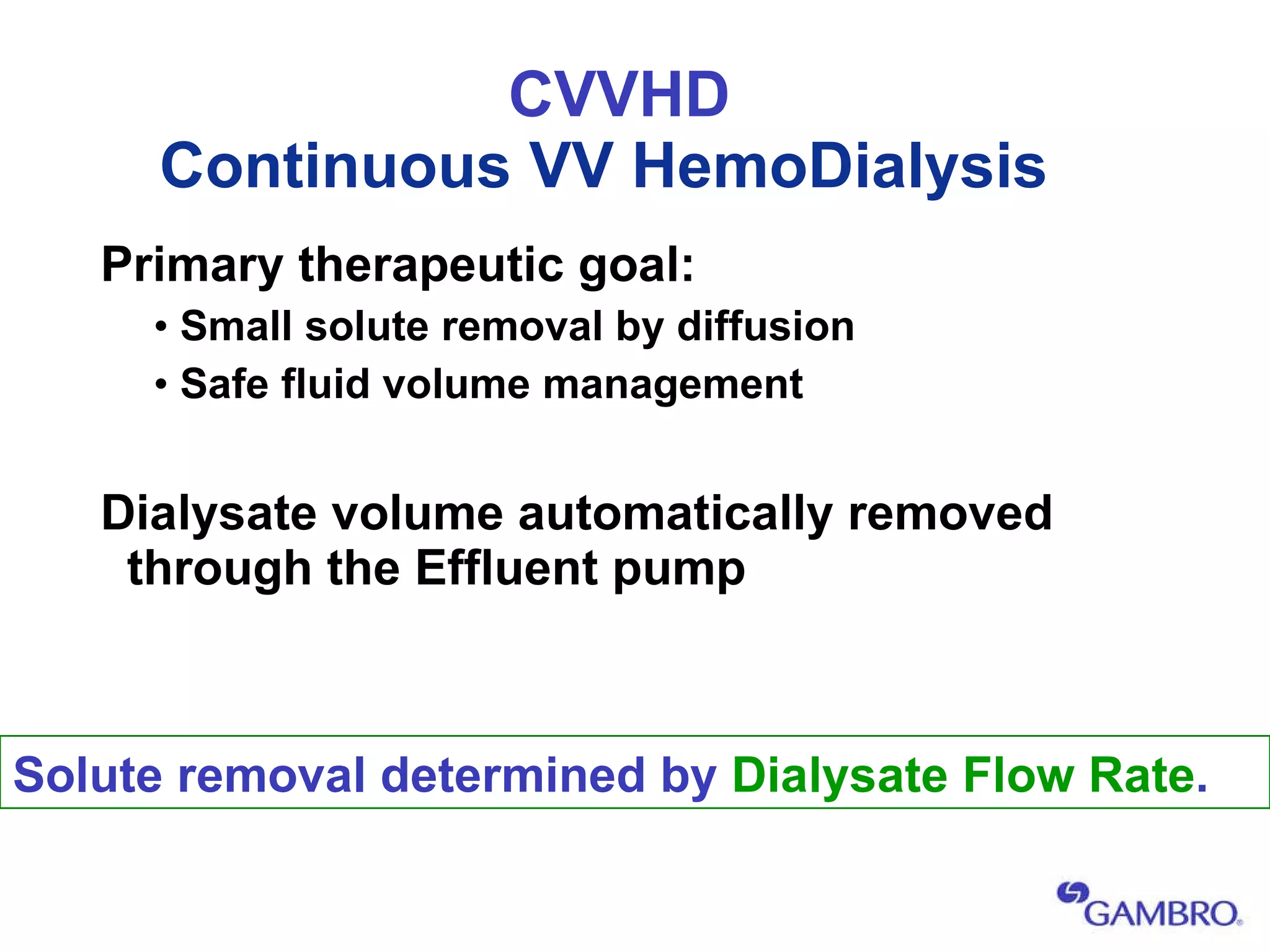
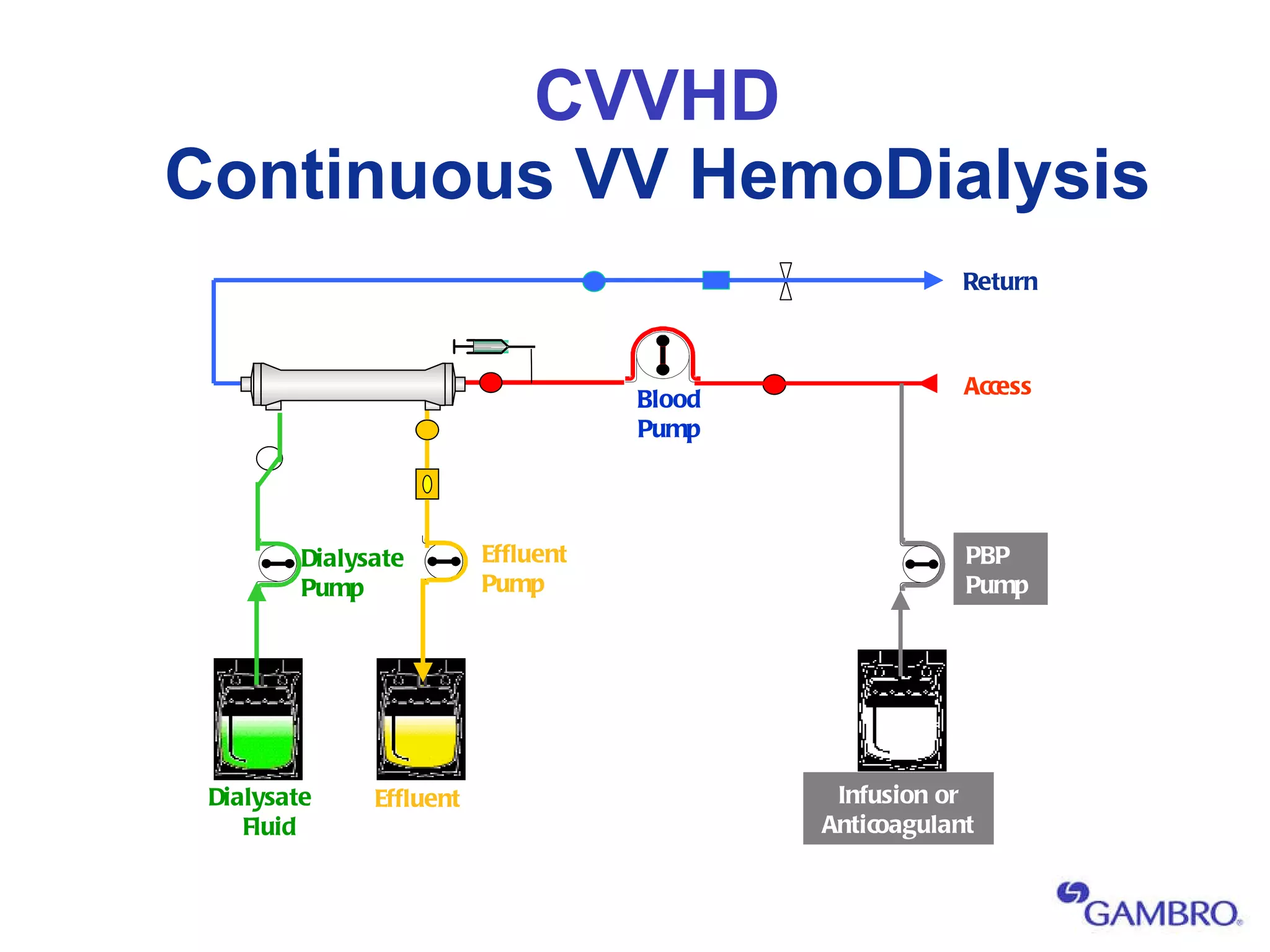
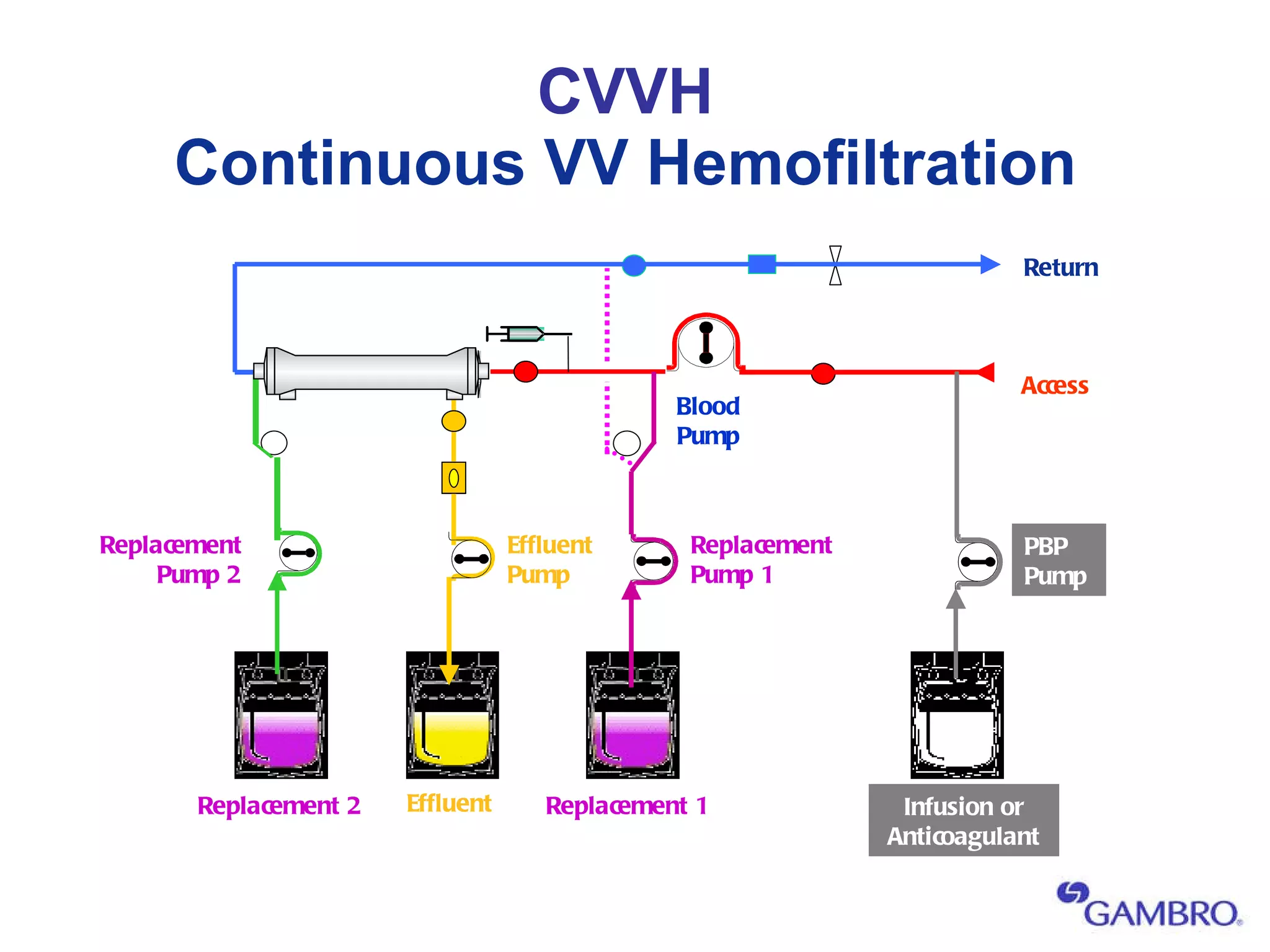
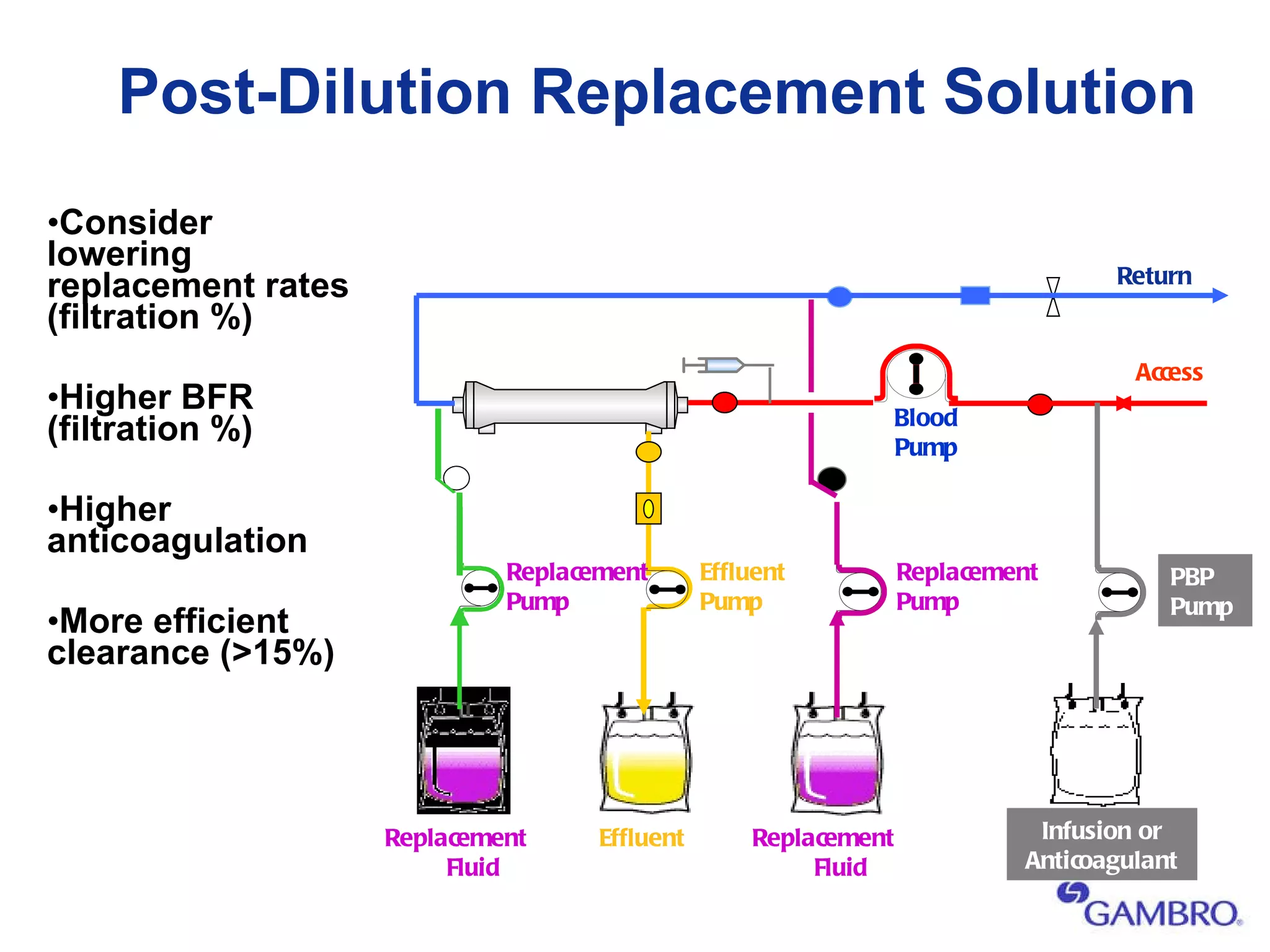
The document outlines the objectives and key concepts of a training course on continuous renal replacement therapy (CRRT). It defines CRRT and discusses the basic principles of CRRT, including solute transport mechanisms, clinical indications, machine setup and safety features, and fluid balance principles. It also summarizes evidenced-based research showing improved patient survival with early CRRT initiation and adequate dose delivery.