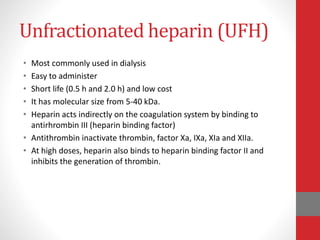
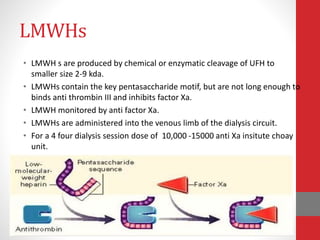
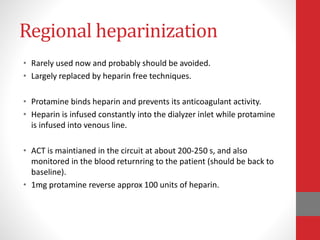
This document discusses anticoagulation during hemodialysis. It begins by explaining coagulation and anticoagulants. Unfractionated heparin is the most commonly used anticoagulant for hemodialysis as it can be administered via infusion pumps and has a short half life. The maintenance dose is monitored via aPTT or ACT tests. Low molecular weight heparins are also used as they have fewer side effects compared to unfractionated heparin. Regional anticoagulation was used in the past but has been replaced by heparin-free techniques due to risks of rebound bleeding.