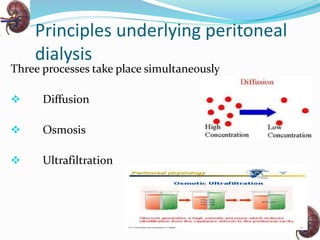
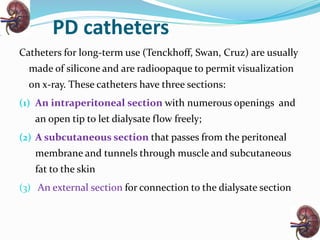
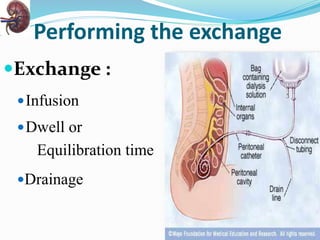
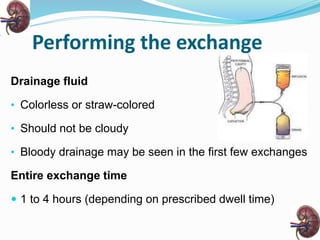
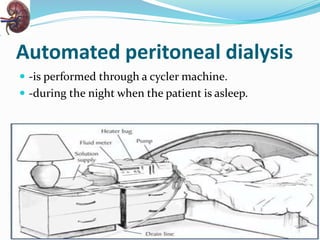
Peritoneal dialysis is a treatment for kidney failure that uses the peritoneal membrane in the abdomen as a filter. It involves infusing dialysate fluid into the abdomen through a catheter for diffusion and osmosis to occur. There are various types of peritoneal dialysis including continuous ambulatory peritoneal dialysis, automated peritoneal dialysis, and intermittent peritoneal dialysis. Nursing management focuses on preventing infections, monitoring for fluid overload, managing pain, and providing education on catheter care and lifestyle adjustments. Peritoneal dialysis offers patients greater independence compared to hemodialysis.