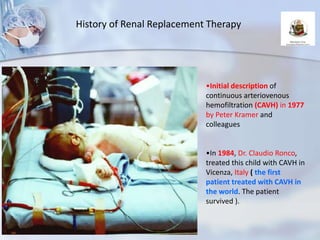
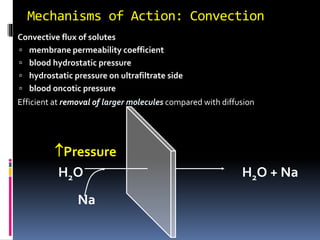
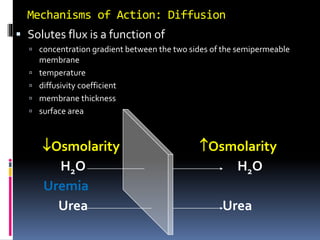
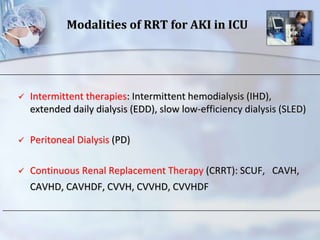
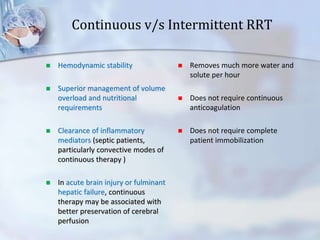
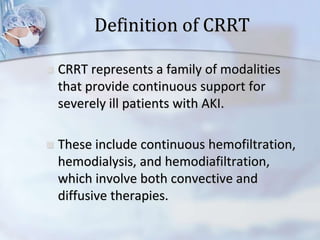
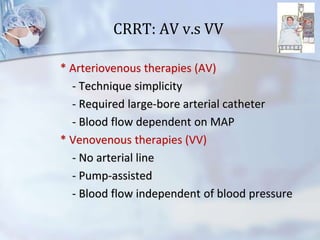
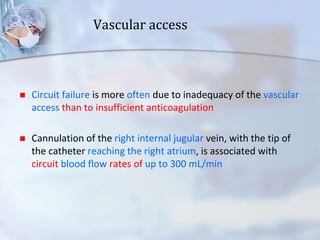
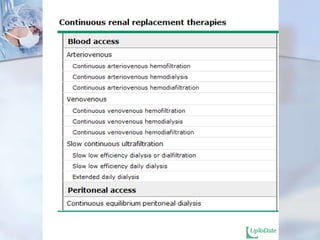
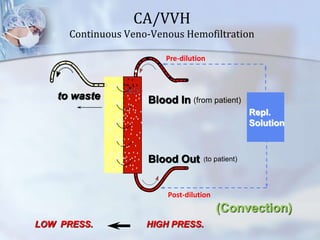
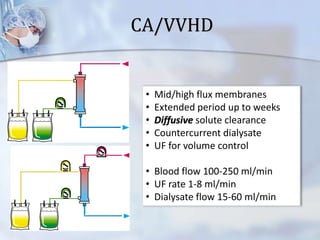
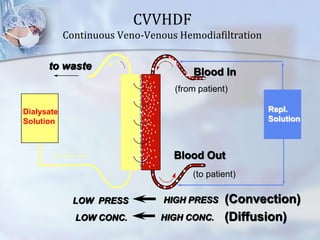
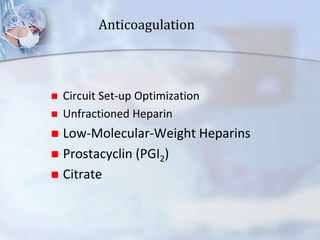
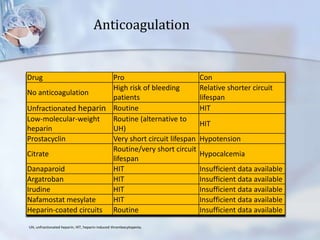
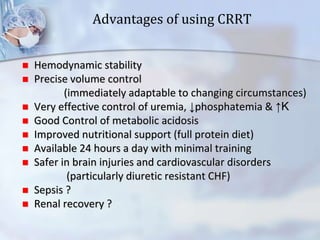
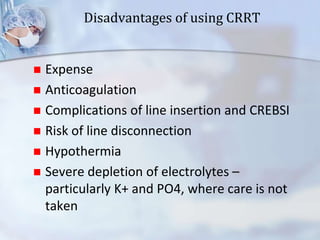
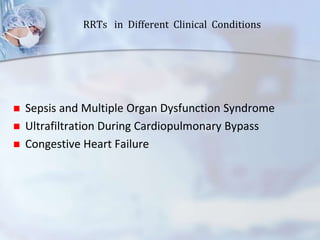
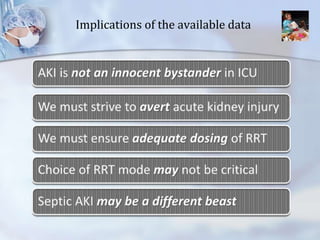
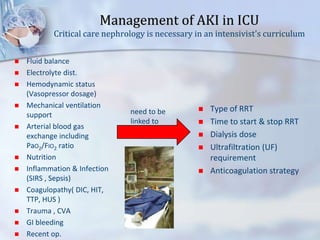
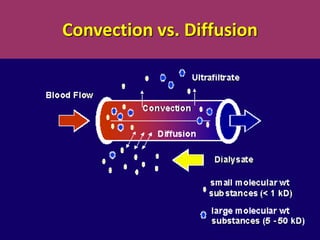
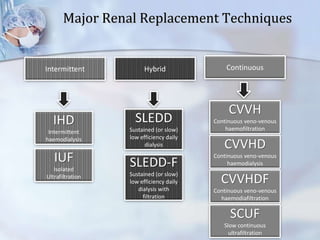
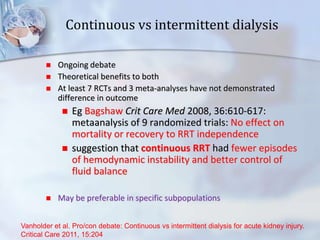
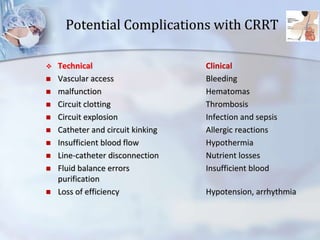
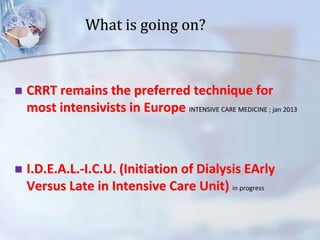
The document discusses continuous renal replacement therapy (CRRT) in critical care units. It begins with definitions and history of renal replacement therapy. It then covers principles, techniques, applications, results and complications of CRRT. The techniques discussed include continuous venovenous hemofiltration (CVVH), hemodialysis (CVVHD) and hemodiafiltration (CVVHDF). Advantages include hemodynamic stability, precise volume control and removal of toxins and cytokines. Complications can include bleeding, infection and electrolyte imbalances. CRRT remains the preferred technique for critically ill patients with acute kidney injury in many intensive care settings.