This document discusses the basic principles of hemodialysis. It covers:
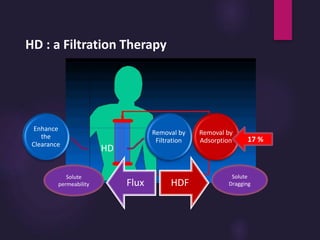
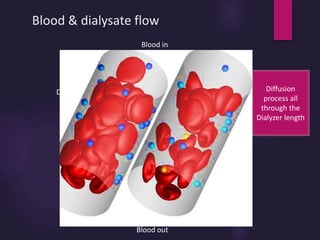
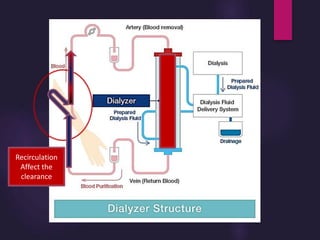
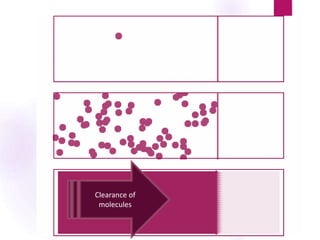
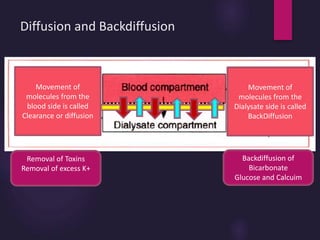
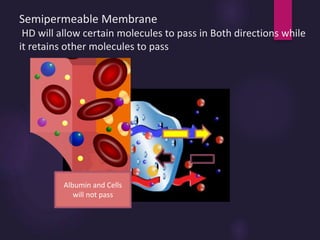
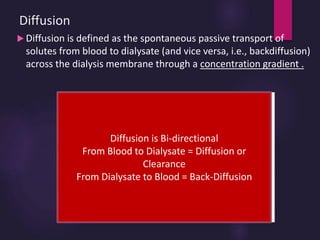
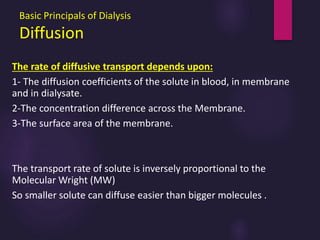
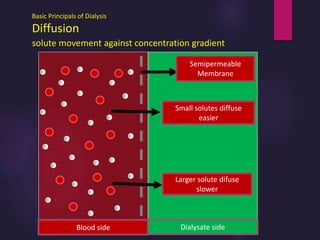
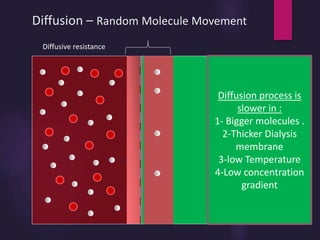
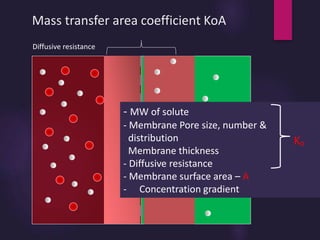
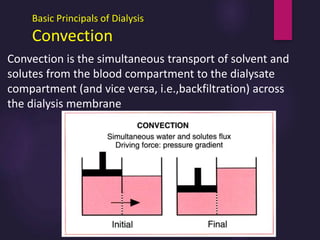
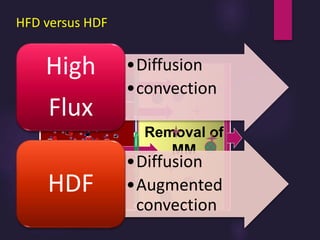
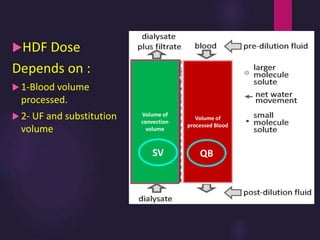
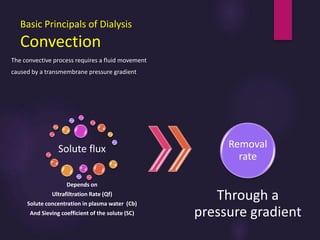
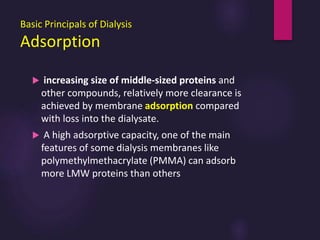
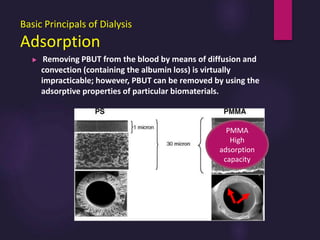
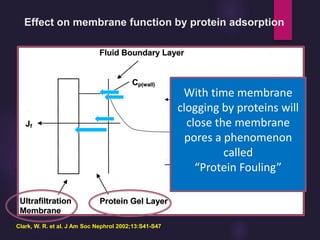
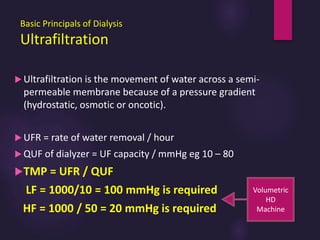
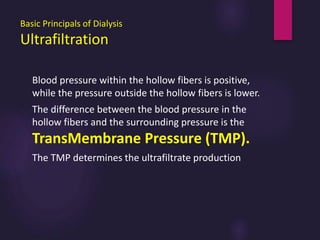
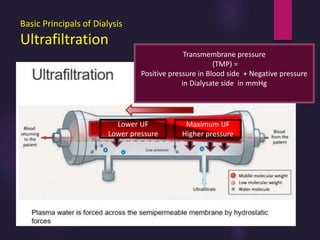
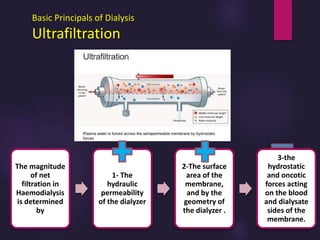
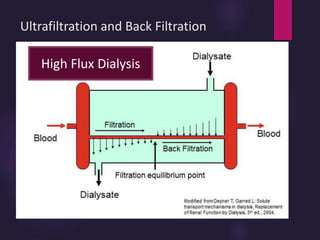
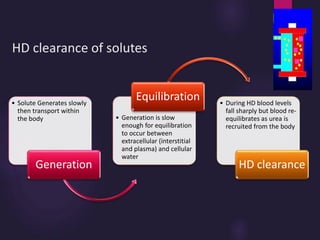
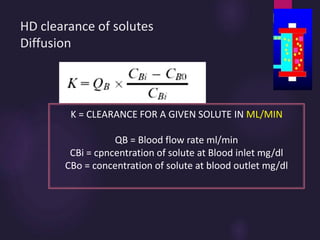
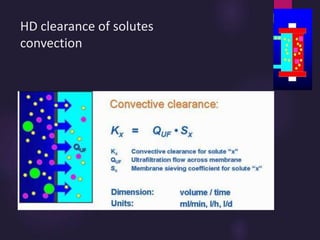
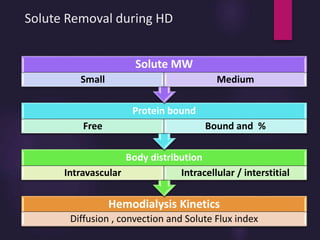
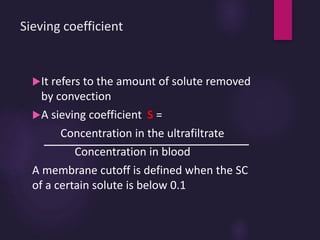
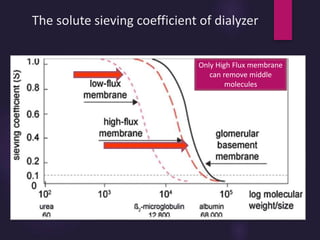
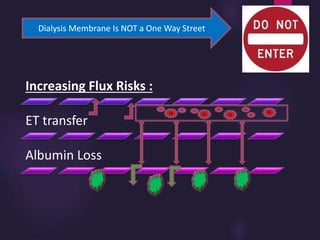
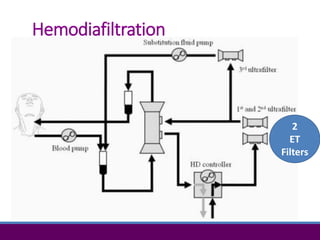
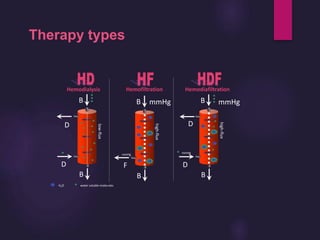
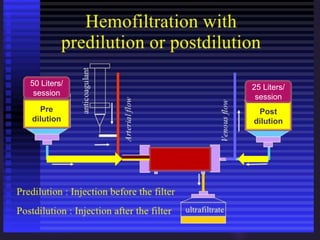
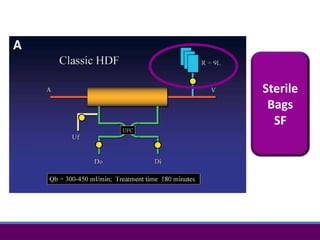
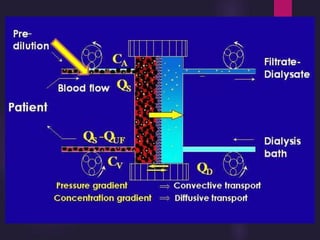
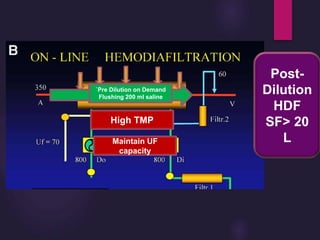
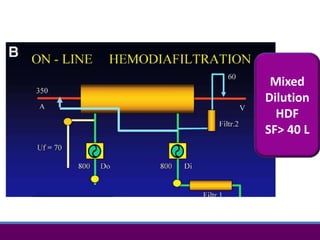
1) Hemodialysis aims to remove waste, correct electrolytes, and remove excess fluids via diffusion, convection, and ultrafiltration across a semi-permeable membrane.
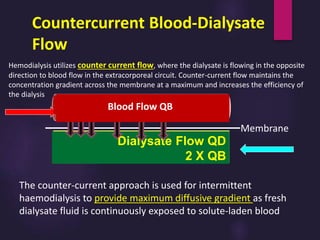
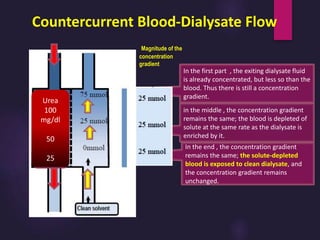
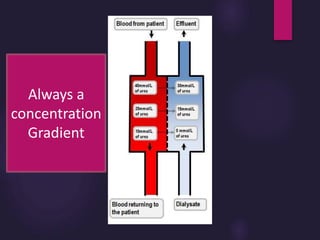
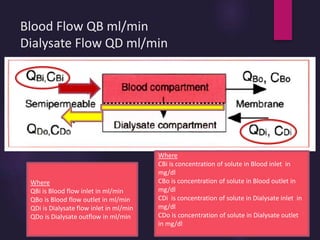
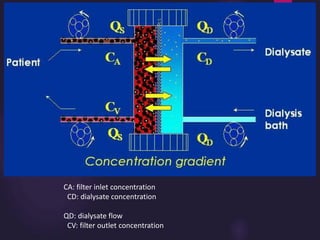
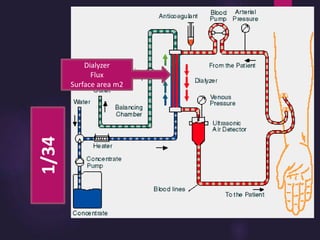
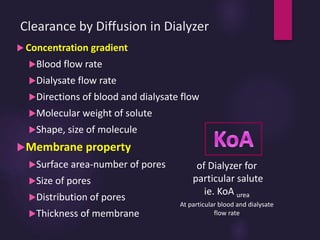
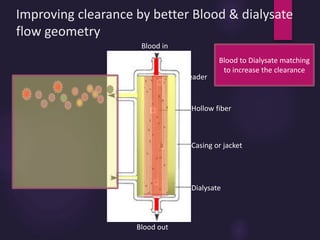
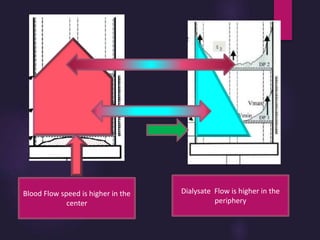
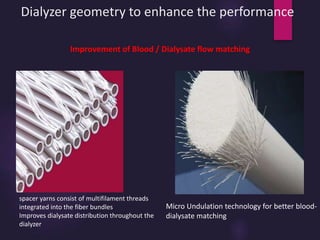
2) Countercurrent blood-dialysate flow maintains the concentration gradient to increase solute removal efficiency.
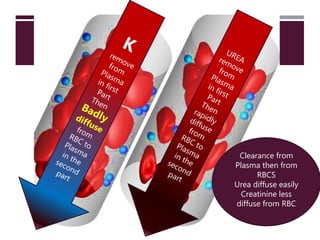
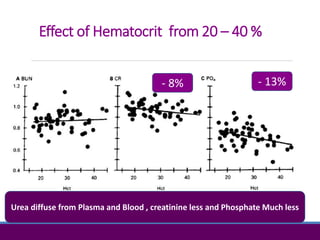
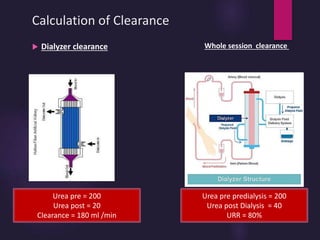
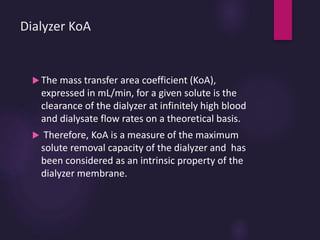
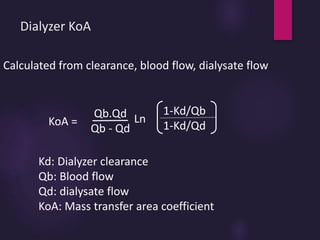
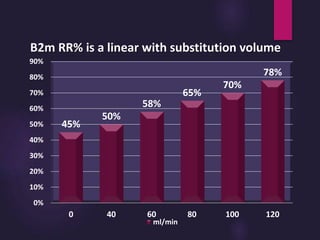
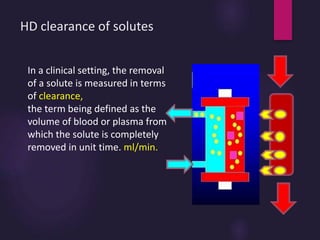
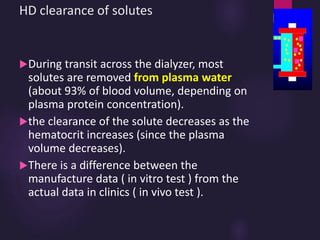
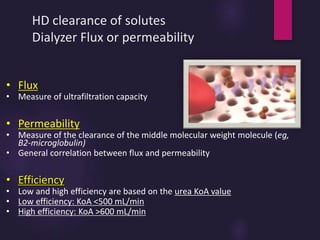
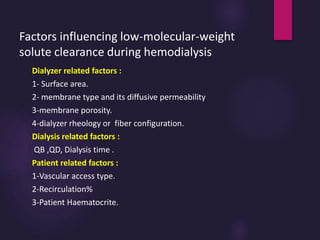
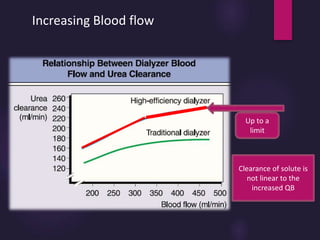
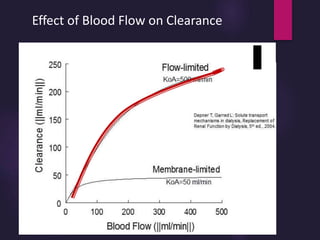
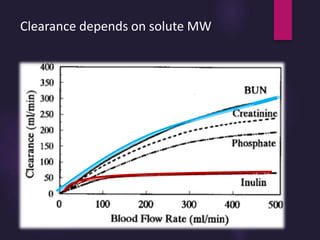
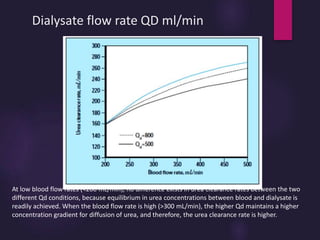
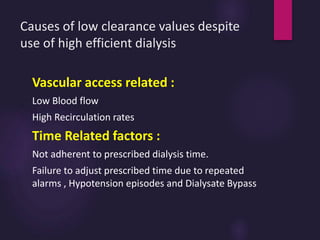
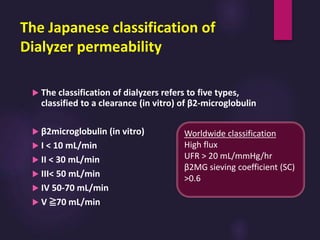
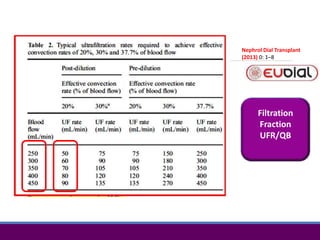
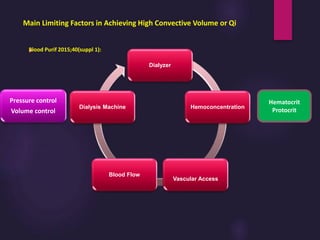
3) Clearance depends on factors like molecular weight, blood/dialysate flow rates, and dialyzer properties. Higher blood flows and matching dialysate flows can improve clearance.