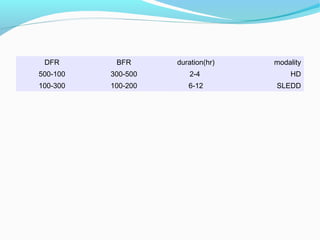
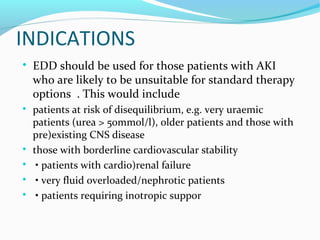
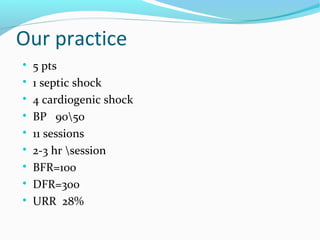
This document discusses sustained low-efficiency daily dialysis (SLEDD) for treating acute kidney injury (AKI) in critically ill patients. SLEDD is a hybrid therapy that combines aspects of continuous renal replacement therapy and intermittent hemodialysis. It allows for a reduced ultrafiltration rate and prolonged treatment duration to maximize dialysis dose while maintaining hemodynamic stability. The document outlines the indications for SLEDD, including patients at risk of disequilibrium or with borderline cardiovascular stability. Preliminary studies suggest SLEDD is a safe and effective option for AKI patients otherwise unsuitable for standard therapies.