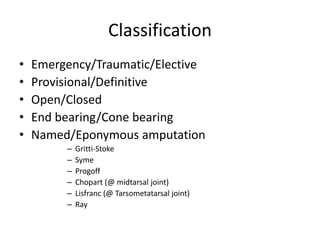
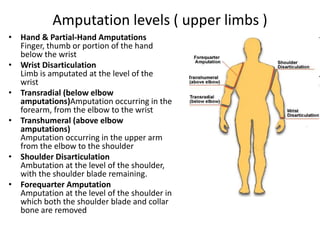
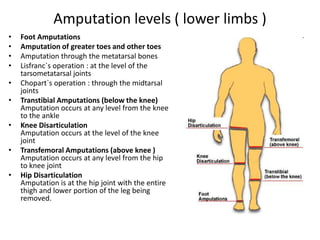
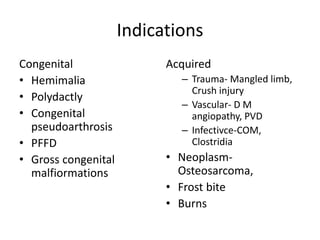
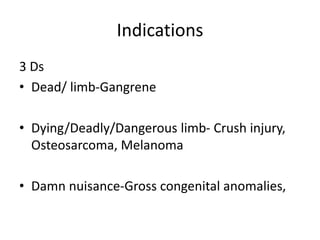
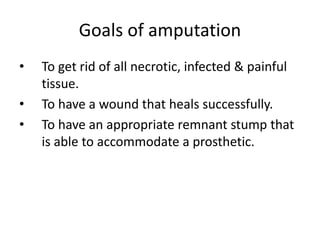
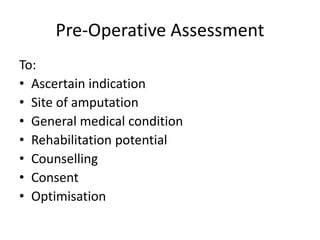
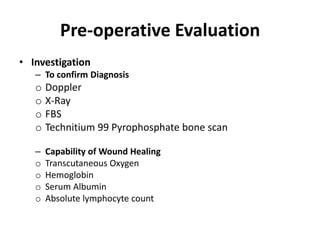
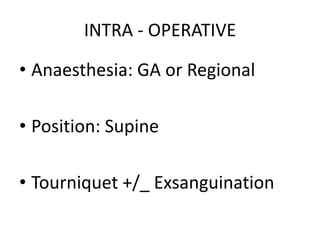
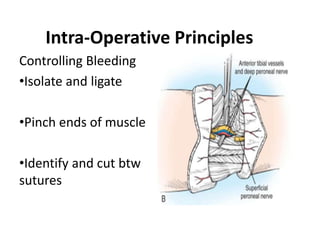
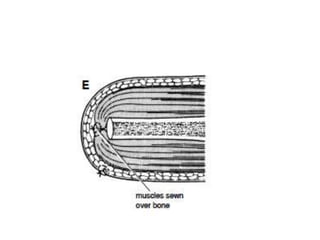
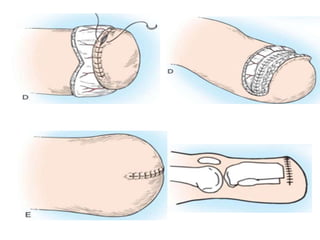
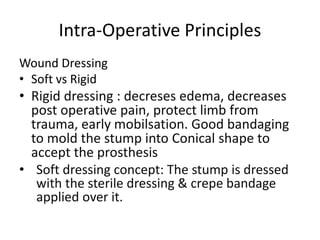
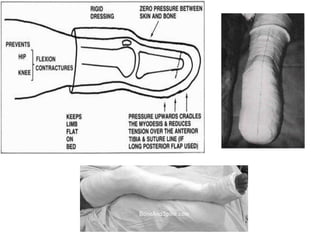
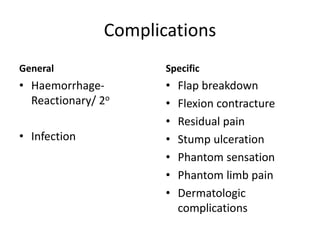
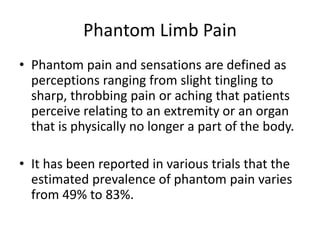
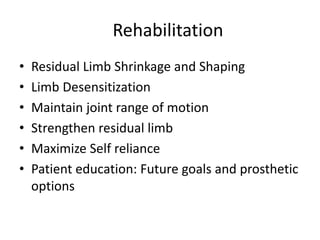
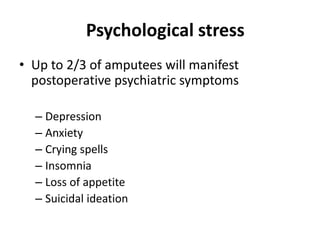
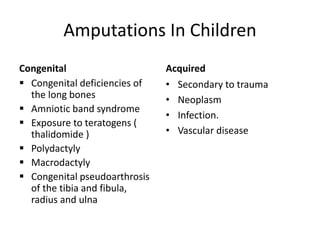
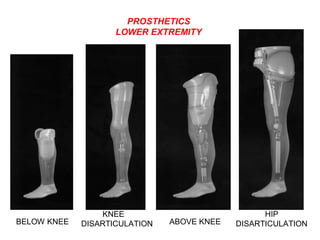
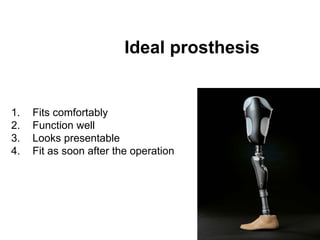
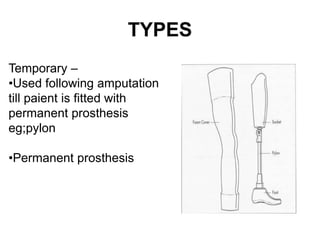
This document outlines principles of amputation, beginning with definitions and a brief history. It discusses indications for amputation including the 3 D's (dead, dying, or damn nuisance limb) and covers pre-operative, intra-operative, and post-operative principles and considerations. Complications are addressed as well as amputation in children. Prosthetics and rehabilitation goals are also summarized. The document provides an overview of best practices and factors to consider for successful amputation outcomes.