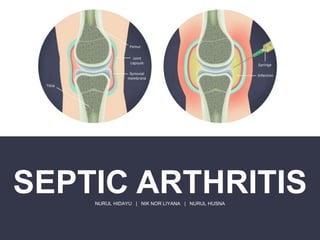
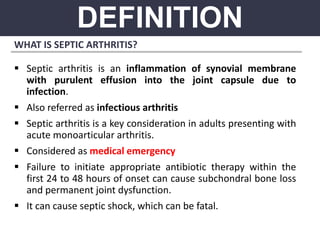
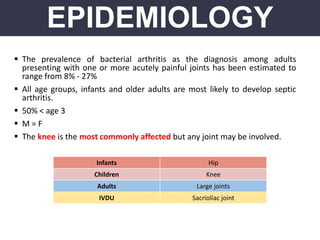
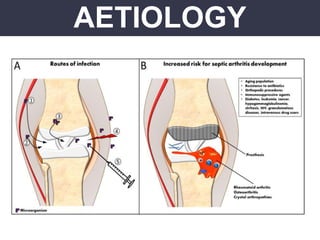
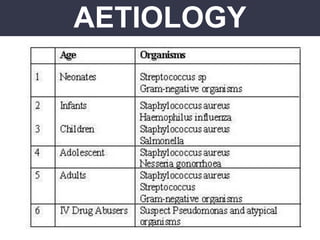
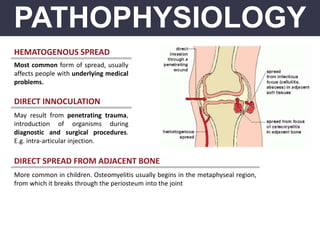
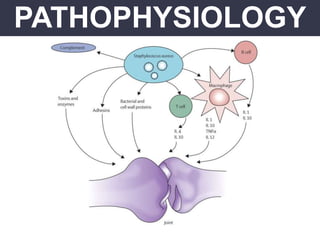
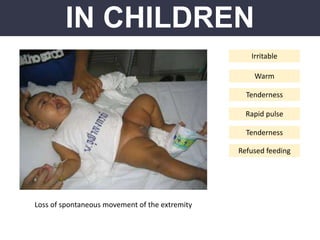
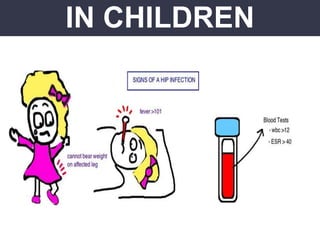
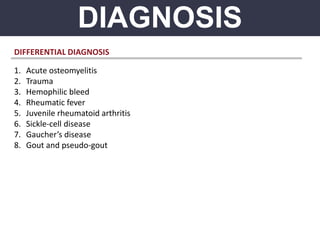
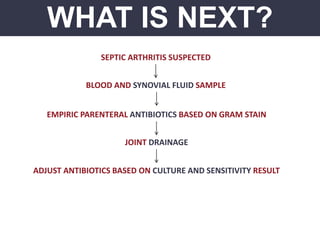
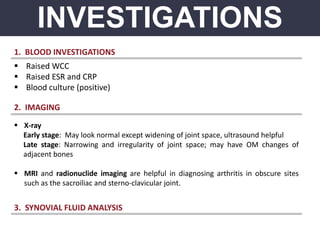
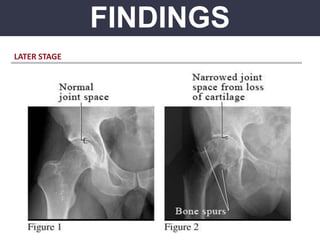
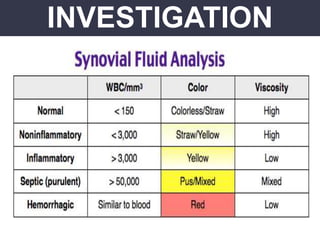
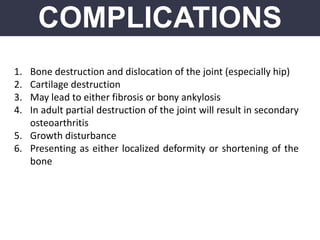
Septic arthritis is an inflammation of the synovial membrane caused by infection, manifesting as a medical emergency typically in cases of acute monoarticular arthritis. Risk factors include age, existing joint problems, immune system weakness, and certain medications, with the knee being the most commonly affected joint. Prompt diagnosis and treatment are crucial to prevent severe complications, including joint dysfunction and systemic infection.