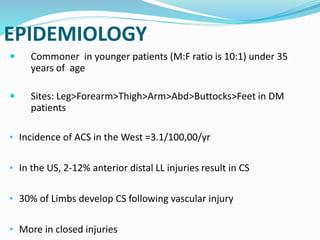
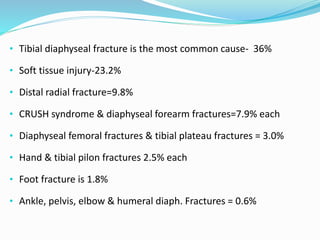
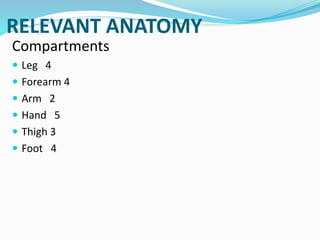
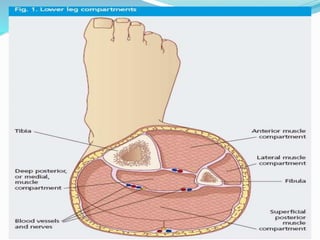
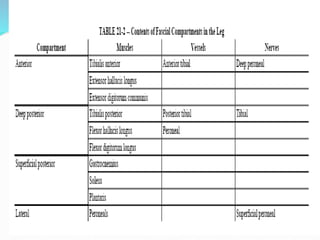
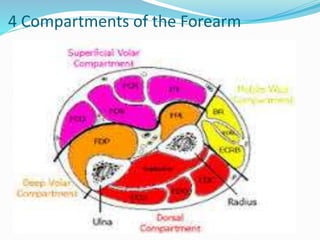
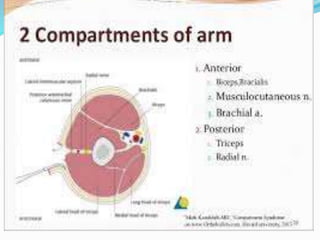
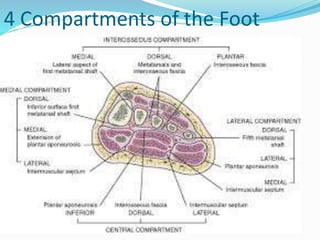
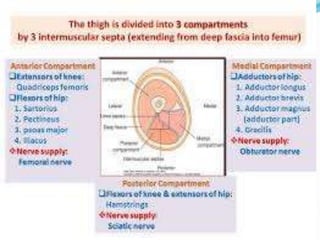
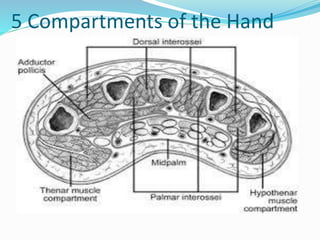
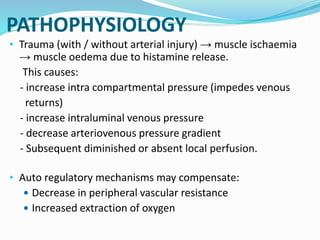
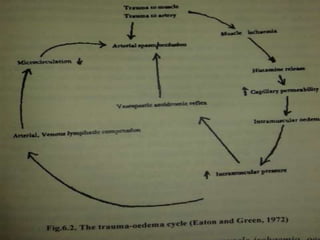
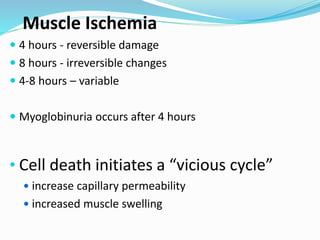
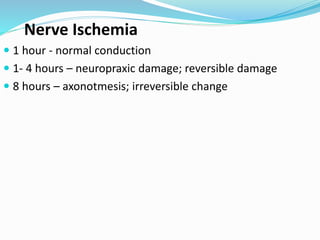
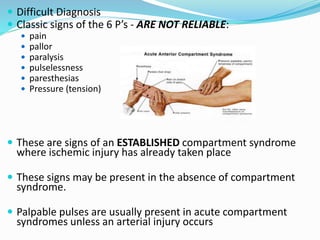
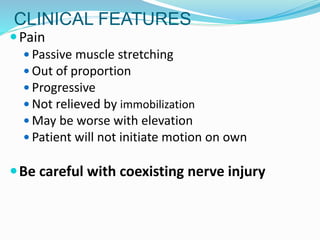
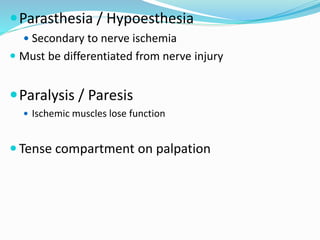
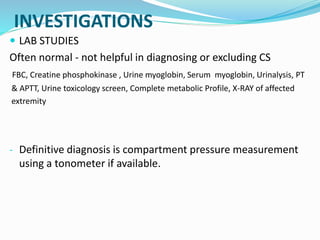
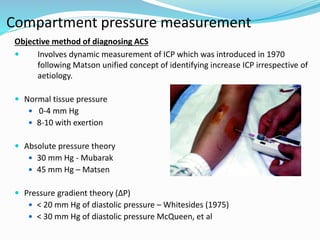
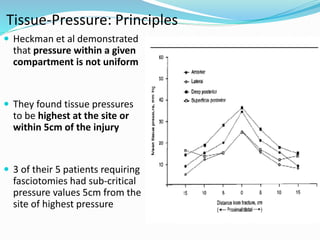
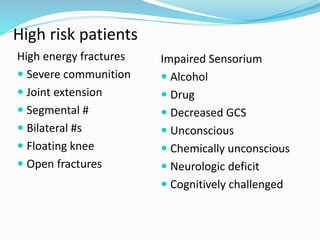
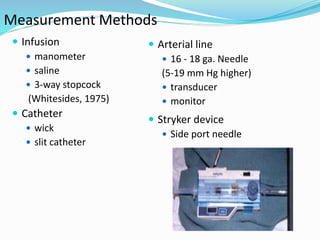
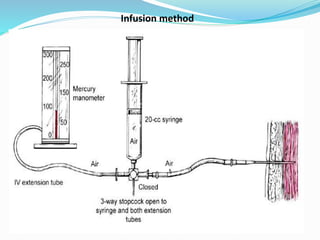
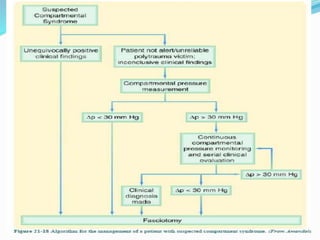
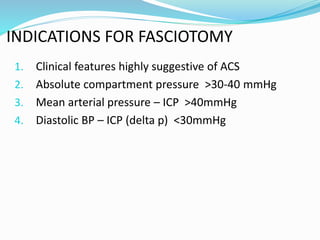
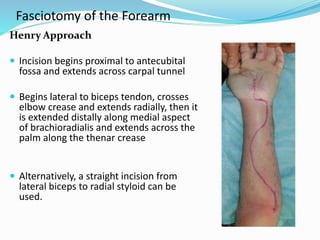
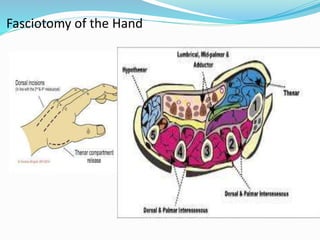
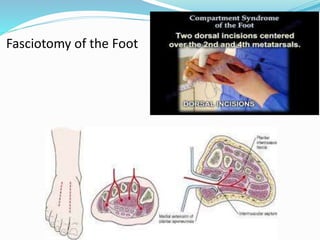
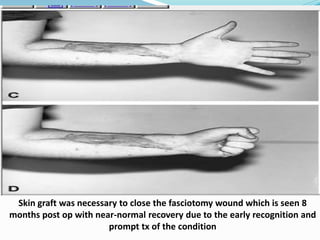
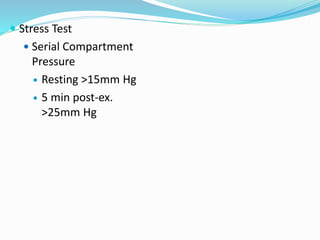
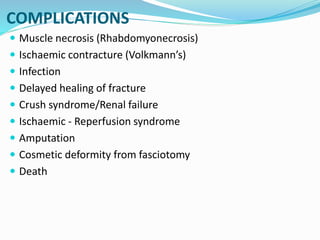
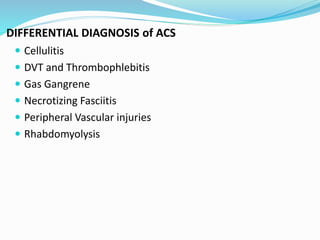
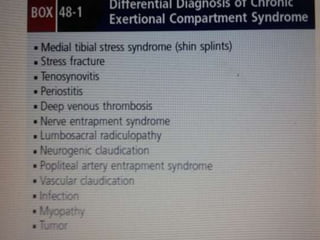
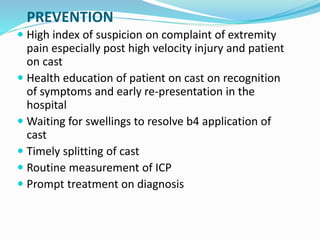
The document discusses compartment syndrome, which is a condition where increased pressure within a limited anatomical space compromises blood circulation and tissue function. It can be acute or chronic depending on cause and duration. The leg and forearm are most commonly affected. After defining the condition and types, the document outlines relevant anatomy, risk factors, pathophysiology, diagnosis including clinical exam and compartment pressure testing, management with fasciotomy, and post-operative care. Compartment syndrome is a surgical emergency if not recognized and treated early through fasciotomy.