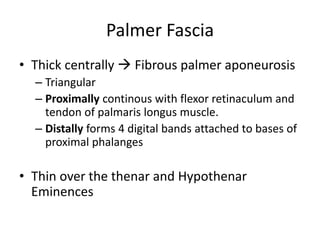
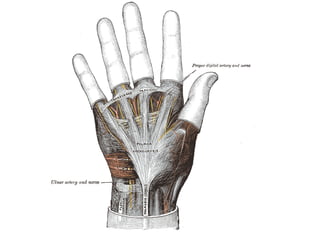
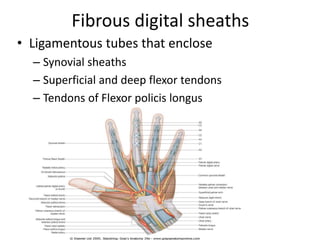
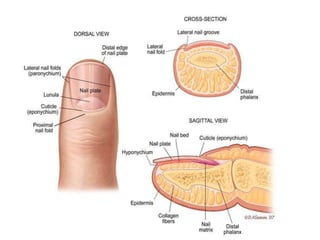
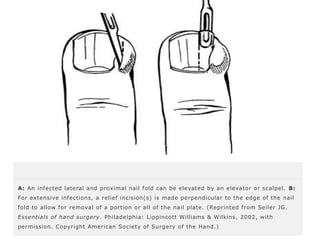
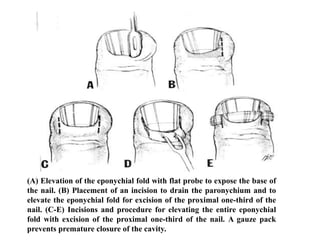
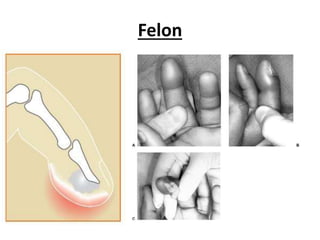
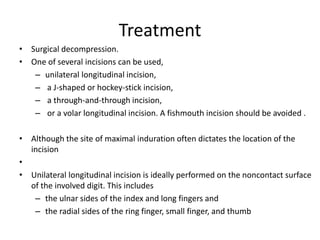
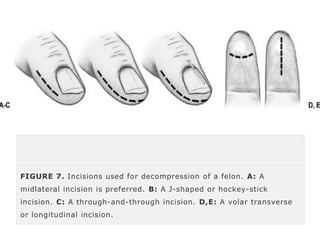
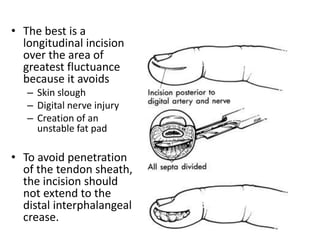
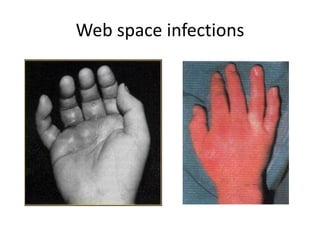
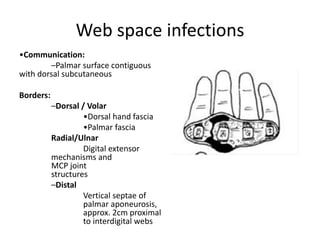
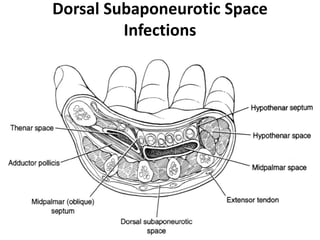
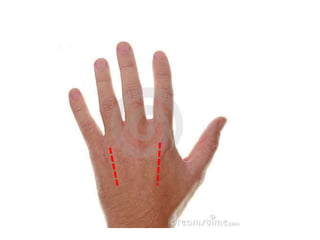
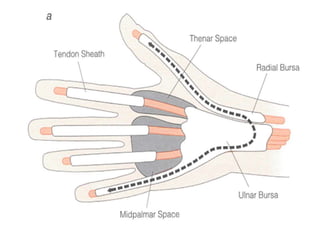
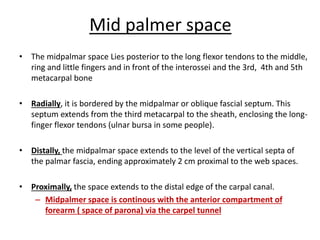
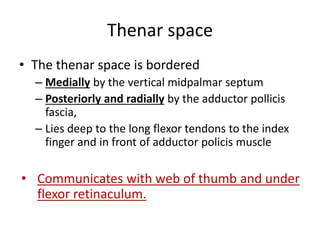
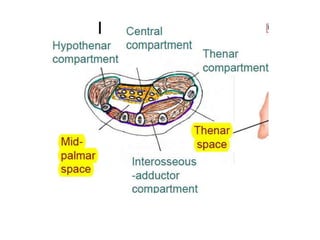
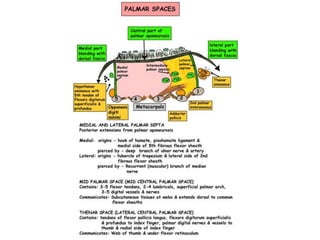
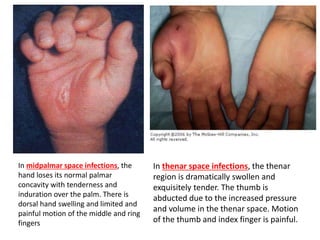
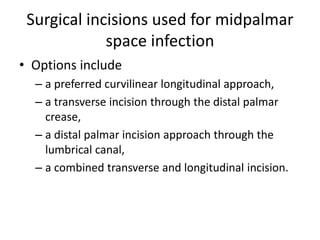
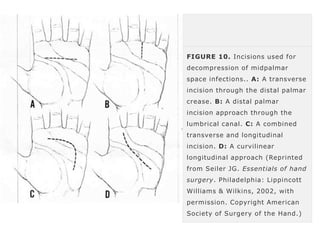
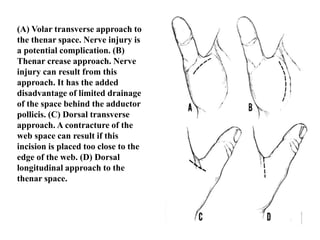
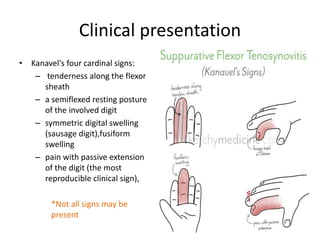
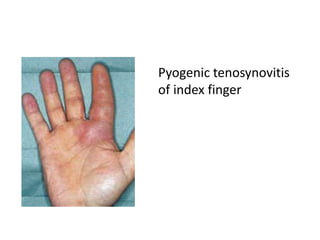
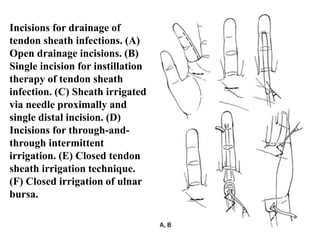
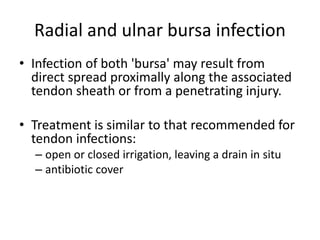
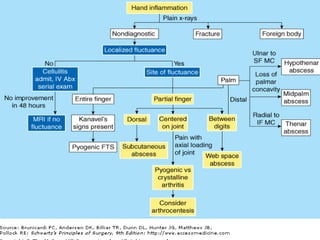
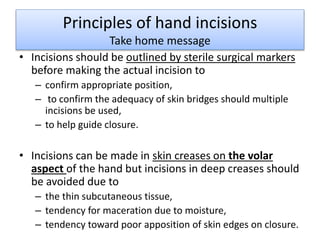
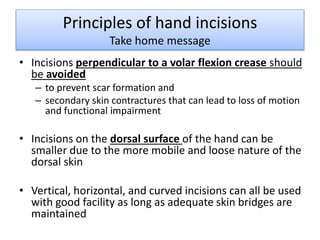
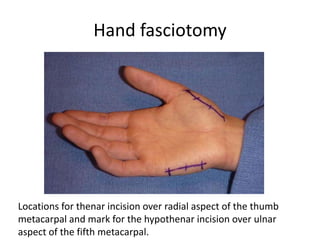
The document provides an overview of various hand infections, focusing on their anatomical basis, clinical significance, and treatment options. It covers conditions such as paronychia, felon, herpetic whitlow, and space infections like midpalmar and thenar space infections, detailing their presentation, pathophysiology, and management strategies. Surgical approaches for drainage and decompression are also highlighted, emphasizing the importance of early treatment to prevent complications.