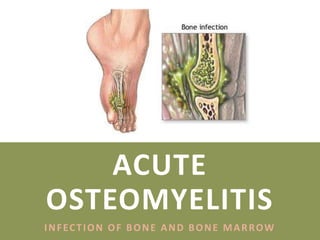
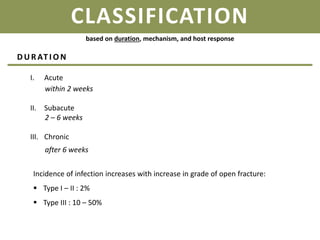
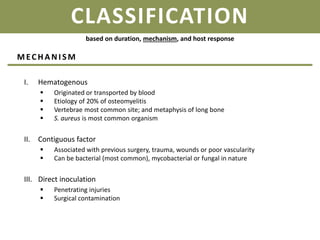
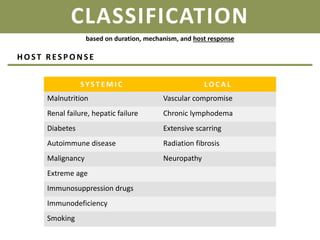
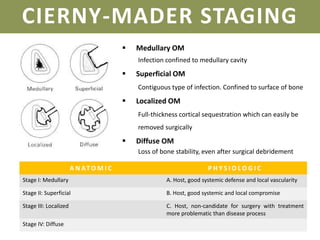
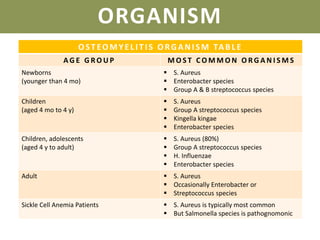
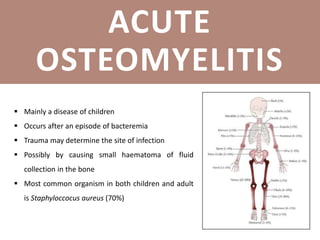
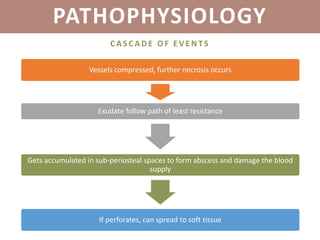
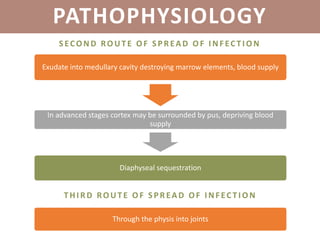
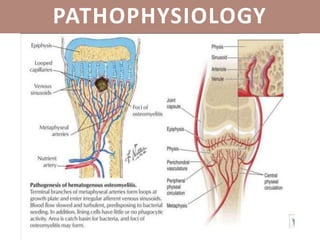
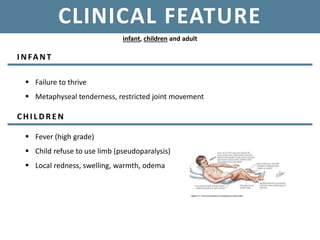
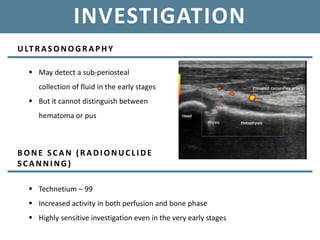
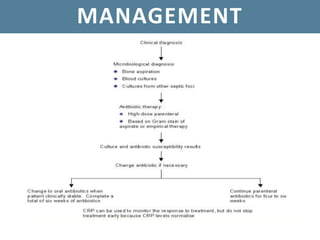
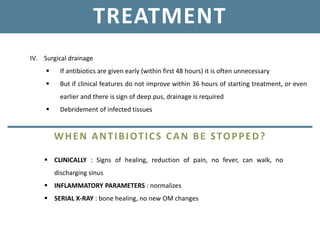
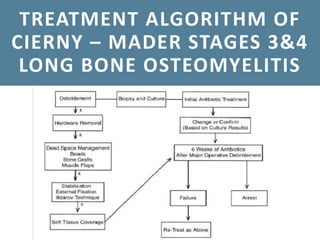
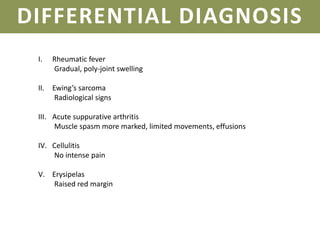
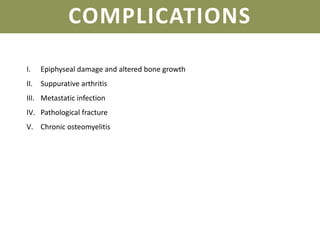
Acute osteomyelitis is a bone and bone marrow infection that can lead to serious complications like osteonecrosis and septic arthritis, primarily affecting children under 5 and adults over 50. The infection can arise from various risk factors, including recent trauma, immunocompromised status, or systemic conditions, and is classified by duration, mechanism, and host response. Diagnosis involves physical examinations and imaging techniques, with management focusing on pain relief, antibiotics, and potentially surgical intervention if there is no improvement.