This document provides information on compartment syndromes, including:
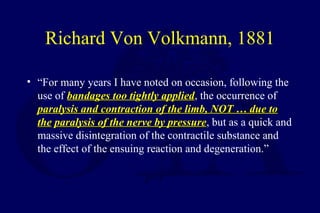
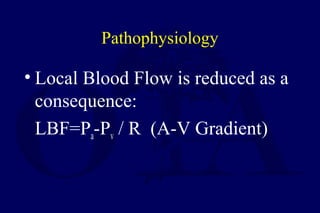
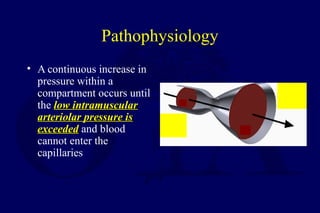
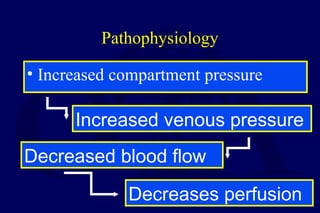
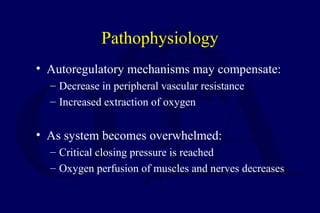
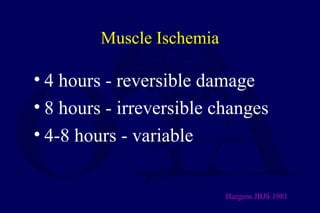
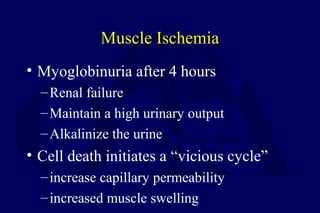
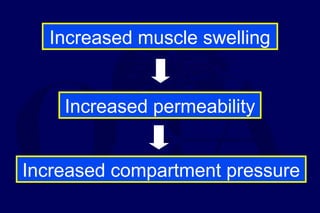
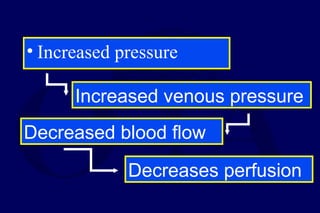
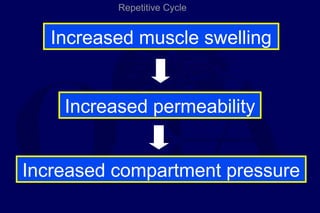
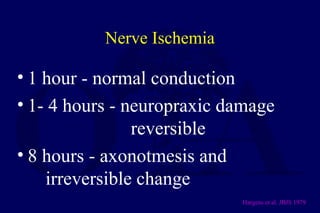
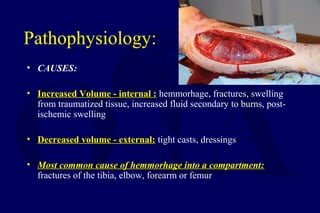
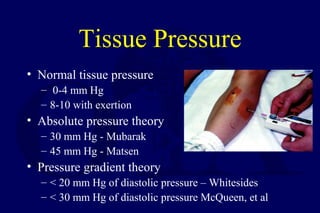
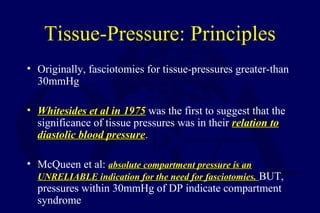
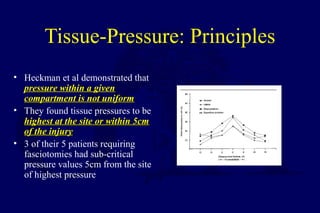
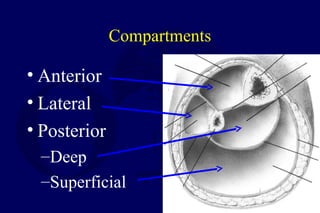
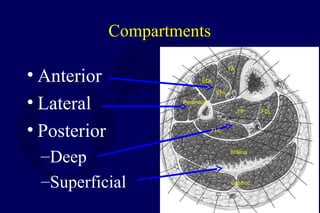
- The pathophysiology of increased pressure within closed muscle compartments leading to reduced blood flow and tissue ischemia.
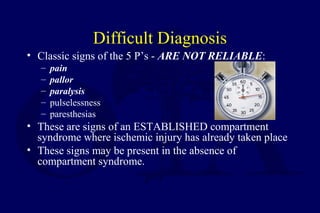
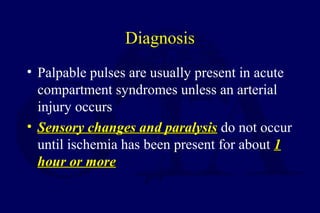
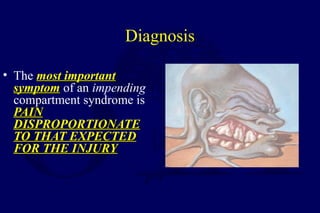
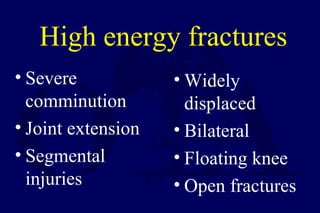
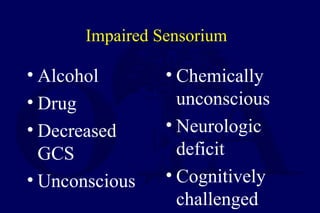
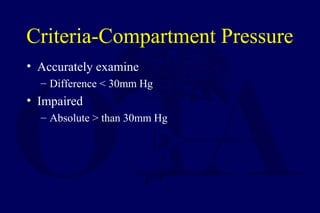
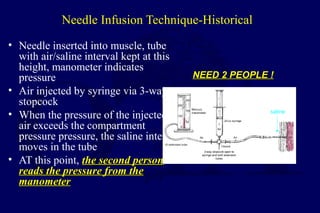
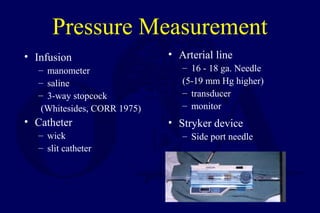
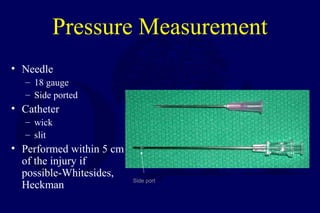
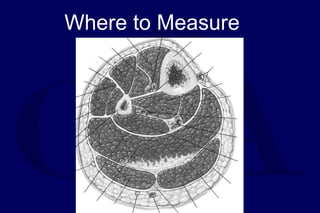
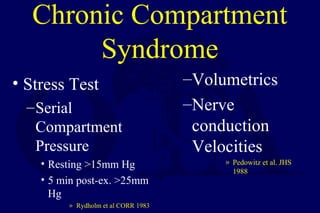
- Risk factors, signs and symptoms including disproportionate pain and elevated compartment pressures measured via needle technique.
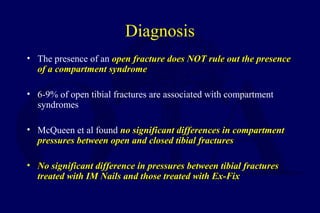
- Diagnosis is clinical with compartment pressures helping to confirm.
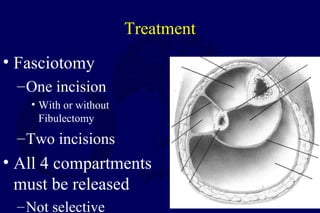
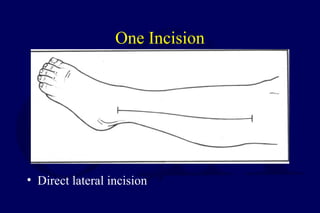
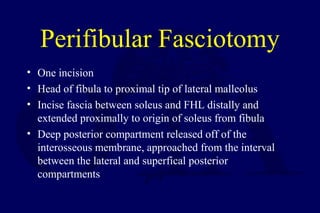
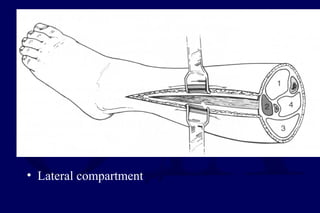
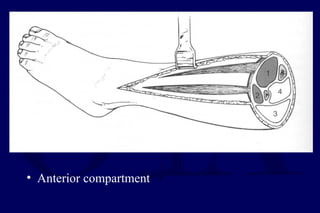
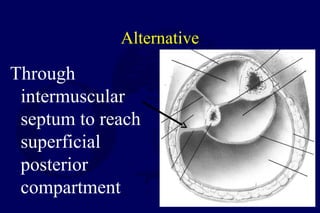
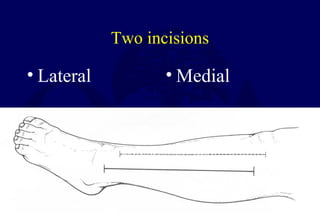
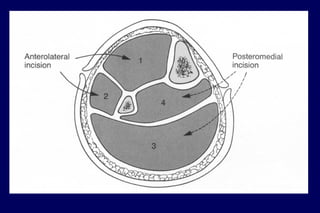
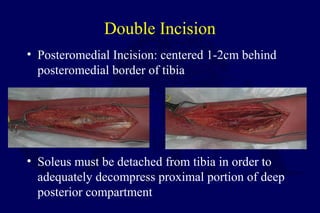
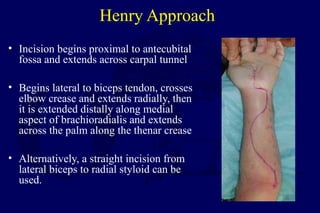
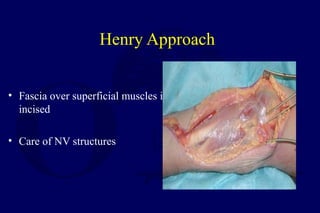
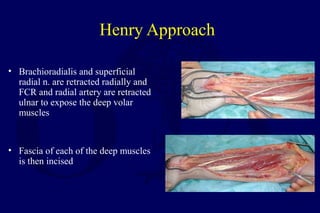
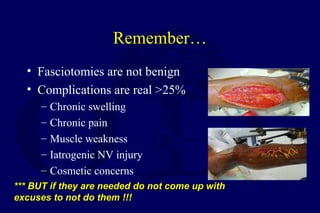
- Treatment involves urgent surgical fasciotomy to decompress all affected compartments before irreversible muscle and nerve damage occurs.
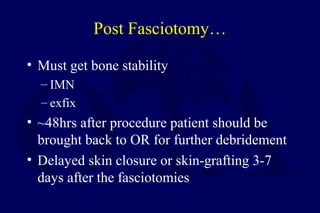
- Post-fasciotomy care and complications are also discussed.