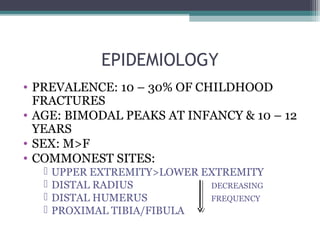
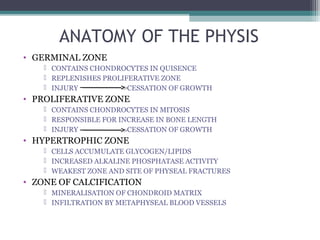
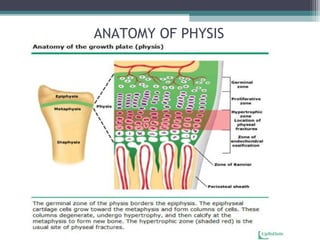
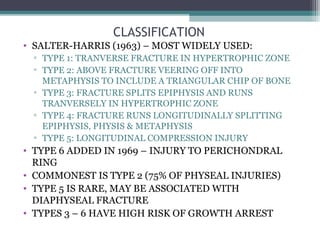
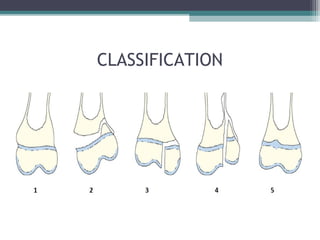
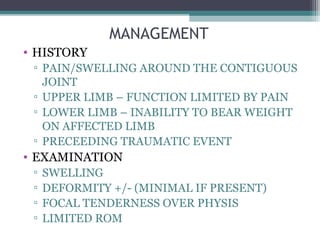
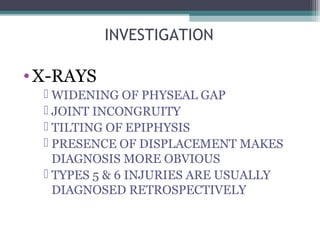
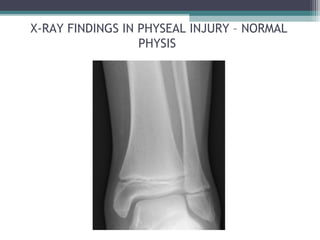
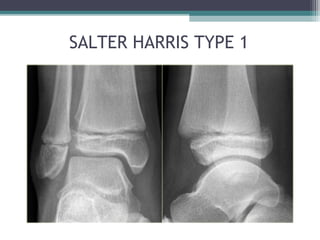
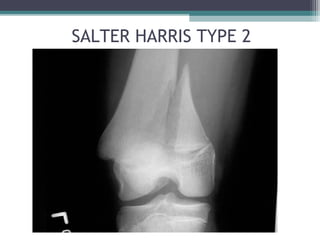
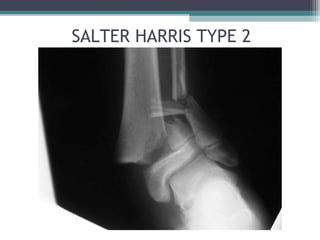
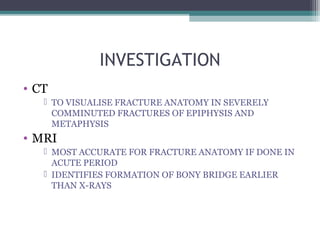
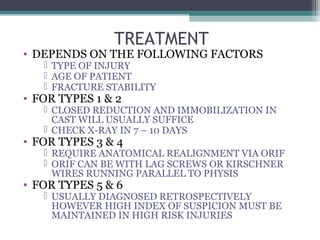
Physeal injuries are disruptions in the cartilaginous physis of long bones, commonly affecting children's growth and quality of life, with a prevalence of 10-30% of childhood fractures. Management of these injuries involves appropriate diagnosis and treatment based on the type and age of the patient, with careful monitoring for potential complications such as growth arrest. Current trends in treatment include the use of gene therapy and tissue engineering to promote healing and prevent complications.