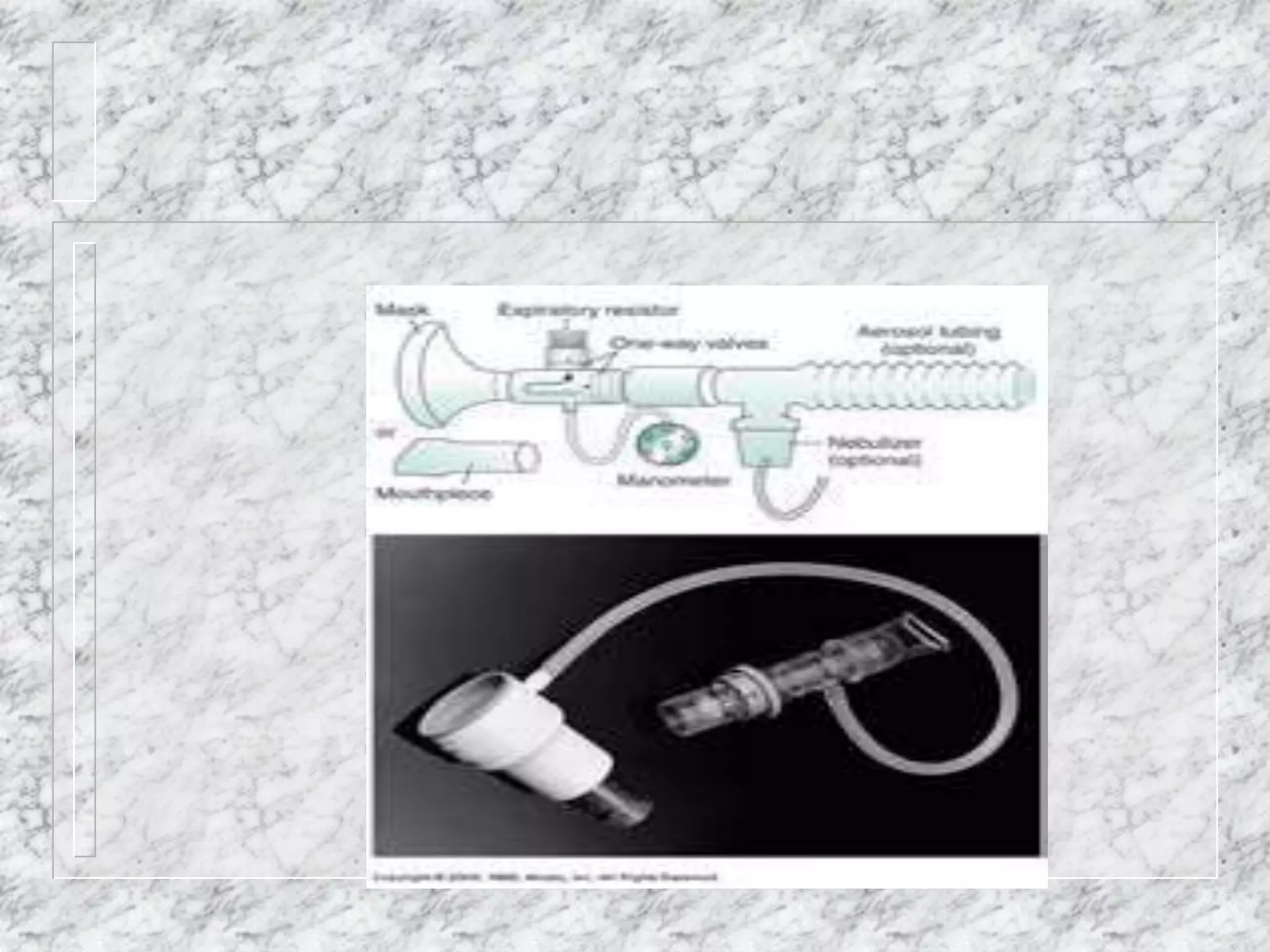
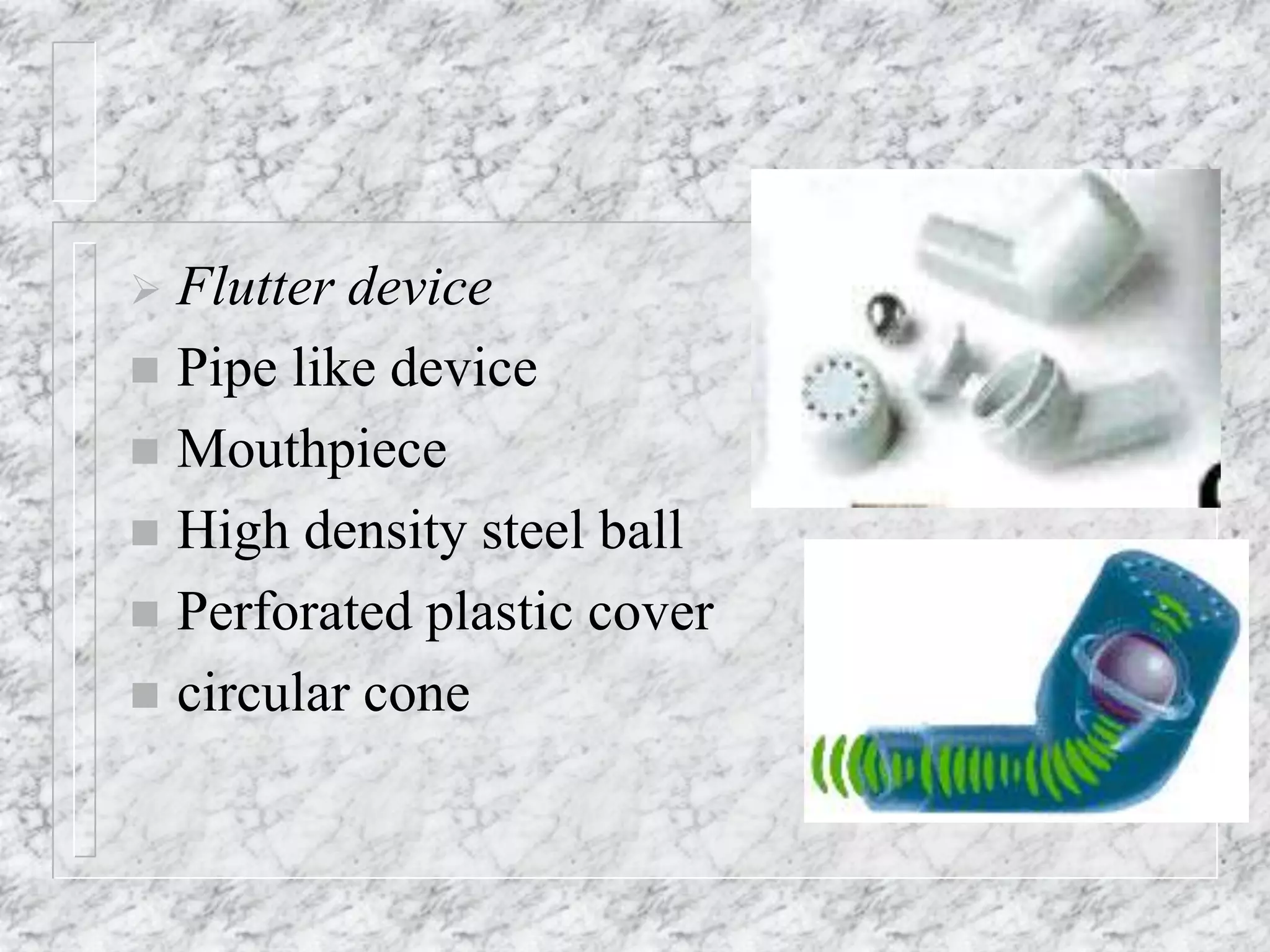
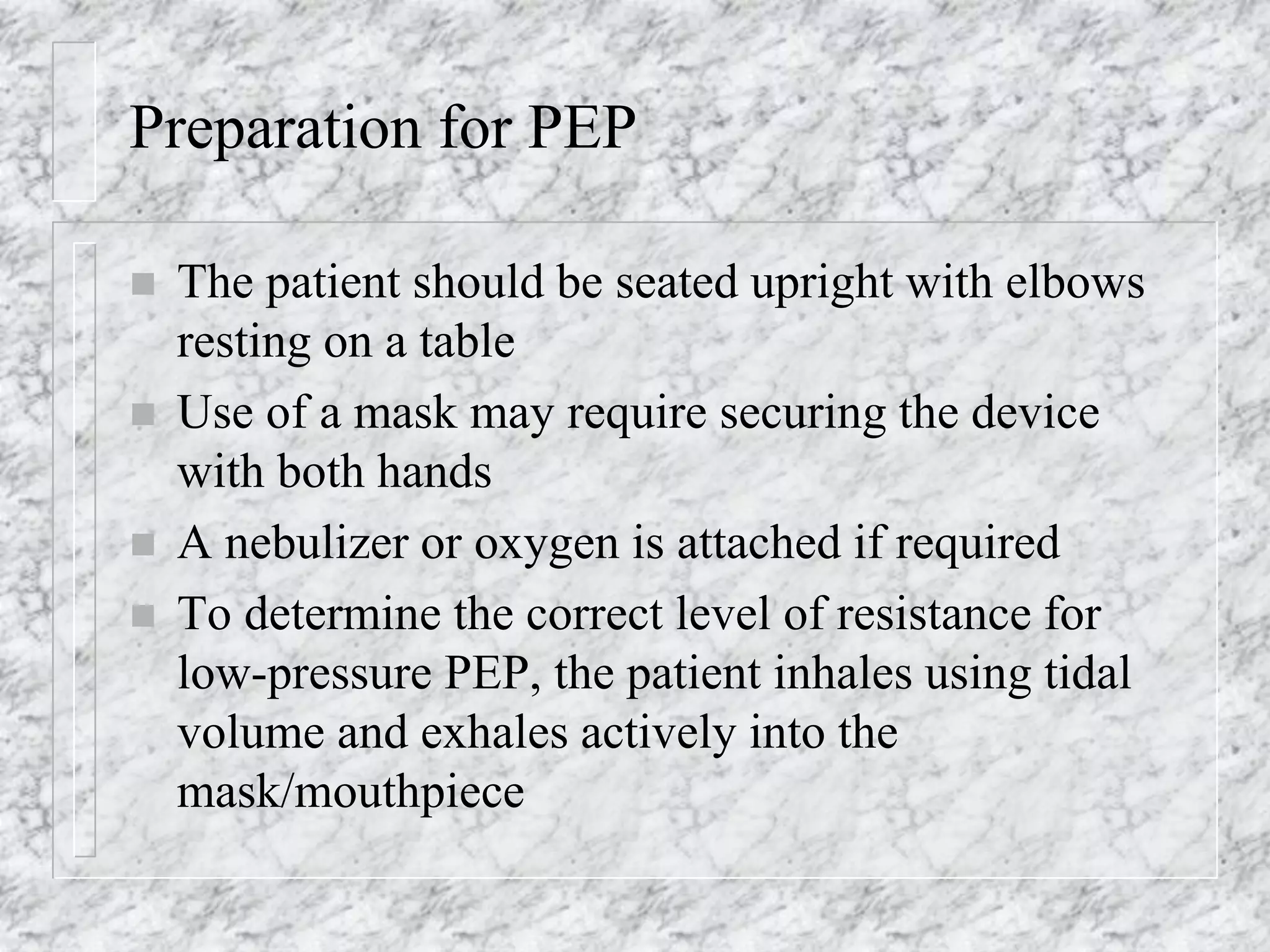
This document outlines various airway clearance techniques designed to improve respiratory function in patients with impaired airway clearance. It discusses the causes and results of ineffective mucociliary clearance, and describes methods such as coughing, postural drainage, active cycle of breathing techniques (ACBT), autogenic drainage, positive expiratory pressure (PEP), suctioning, and high-frequency chest compression (HFCC). These techniques aim to enhance mucus mobilization, reduce lung tissue damage, and improve oxygenation and quality of life.