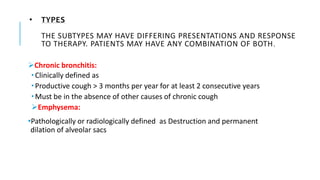
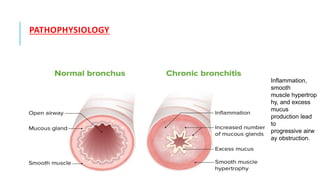
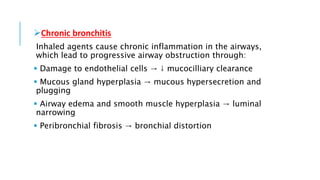
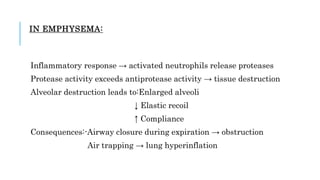
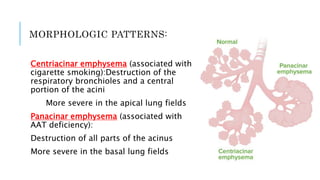
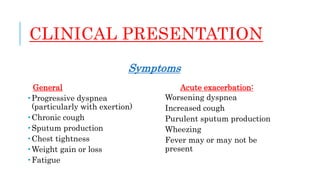
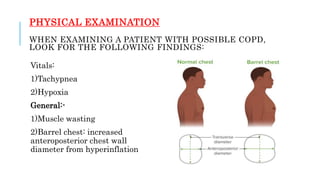
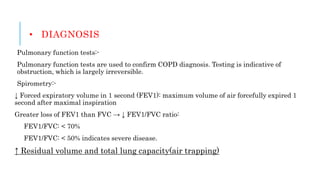
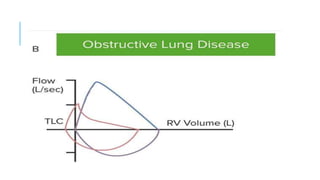
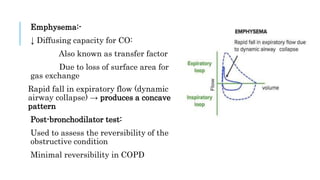
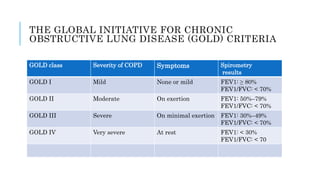
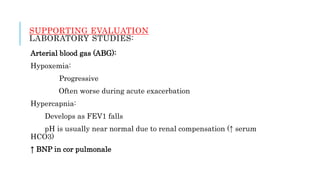
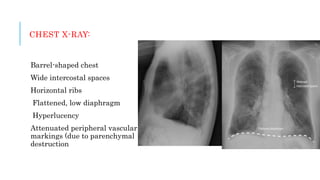
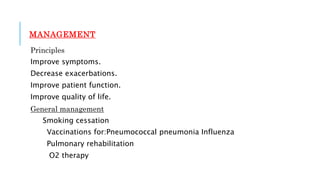
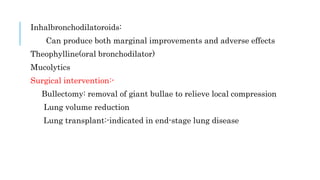
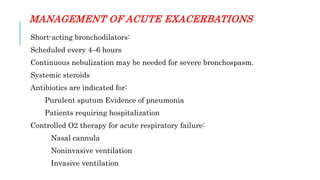
COPD is characterized by airflow limitation caused by airway disease and lung destruction. It includes chronic bronchitis and emphysema. Symptoms include dyspnea, cough, and sputum production. Diagnosis is confirmed by spirometry showing reduced FEV1/FVC ratio. Treatment focuses on smoking cessation, vaccinations, pulmonary rehabilitation, bronchodilators, and corticosteroids to improve symptoms and quality of life. Acute exacerbations are managed with bronchodilators, steroids, and antibiotics. Differential diagnoses include asthma, bronchiectasis, pulmonary embolism, and cystic fibrosis.