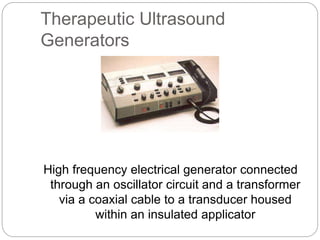
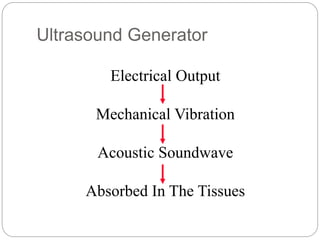
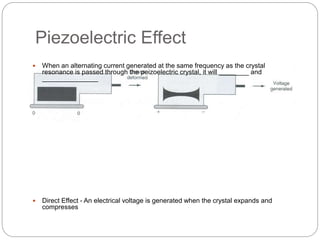
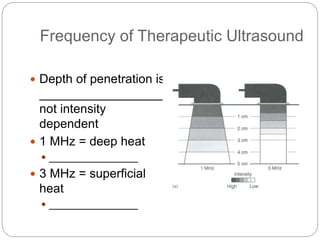
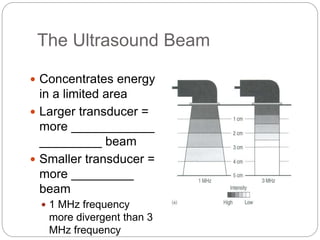
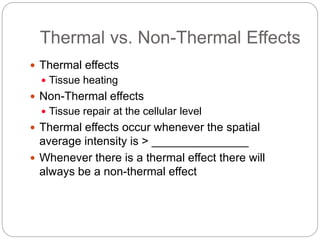
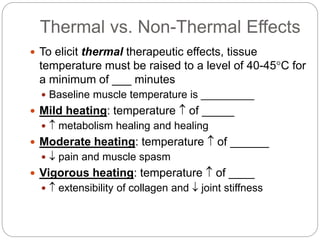
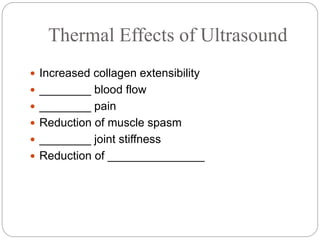
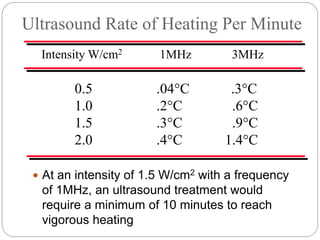
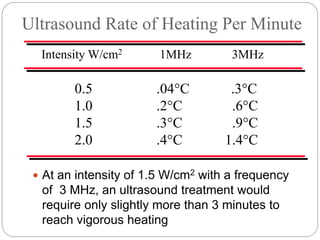
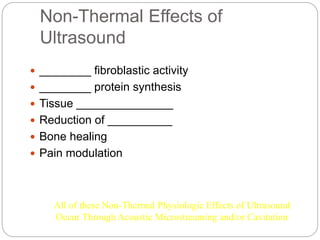
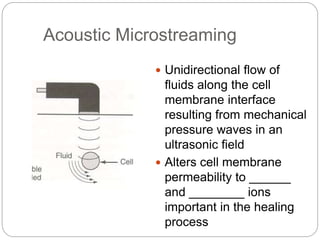
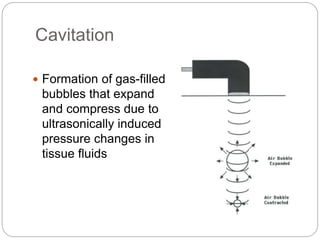
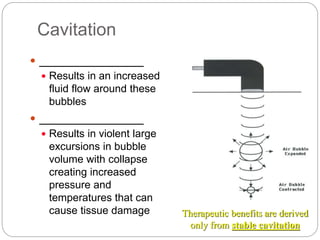
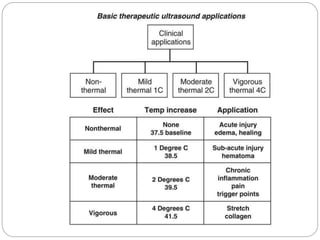
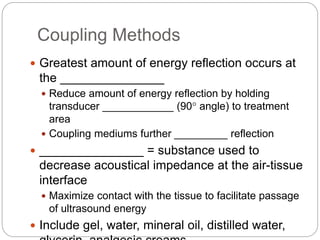
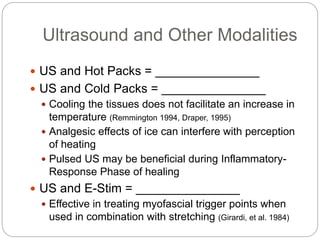
Therapeutic ultrasound is a commonly used modality in sports medicine that produces acoustic vibrations for thermal and non-thermal effects. It utilizes a transducer to convert electrical energy into ultrasound waves, affecting tissue depth and heating depending on frequency. Clinical applications include soft tissue healing, bone repair, and potential use in drug delivery through phonophoresis.